It started with my regular bloodwork for my
semi-annual
check-up in July. Nowadays, you can
download your results and look it over before even seeing the doctor,
which I did. Most everything was in the
green—my cholesterol
is always marginal, but isn’t it for everyone.
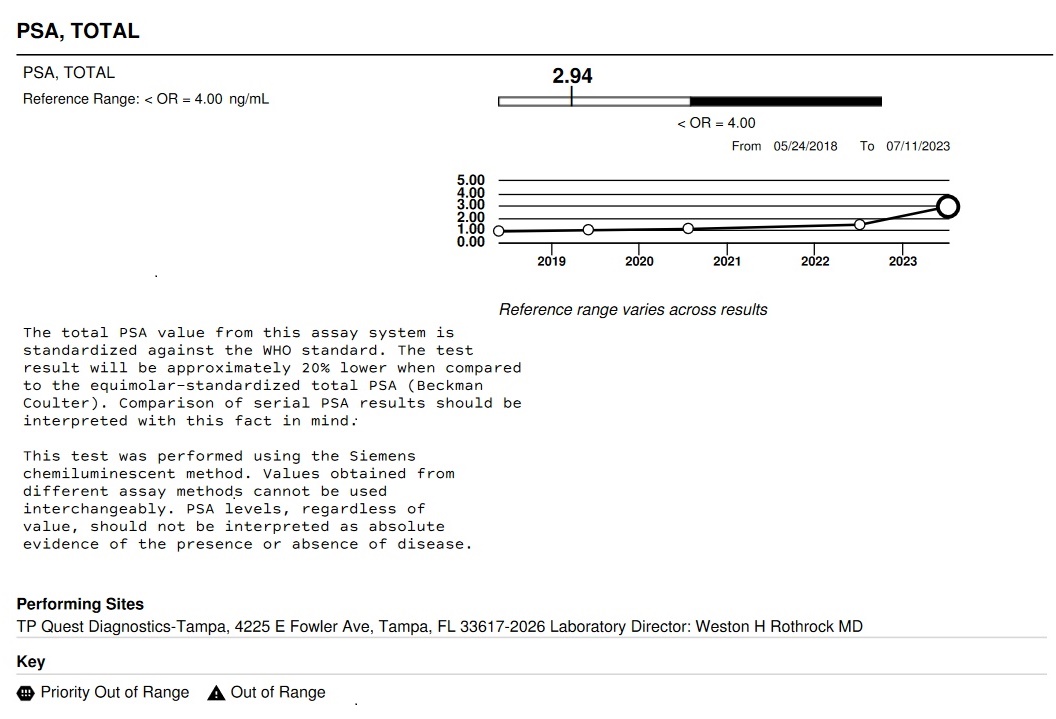
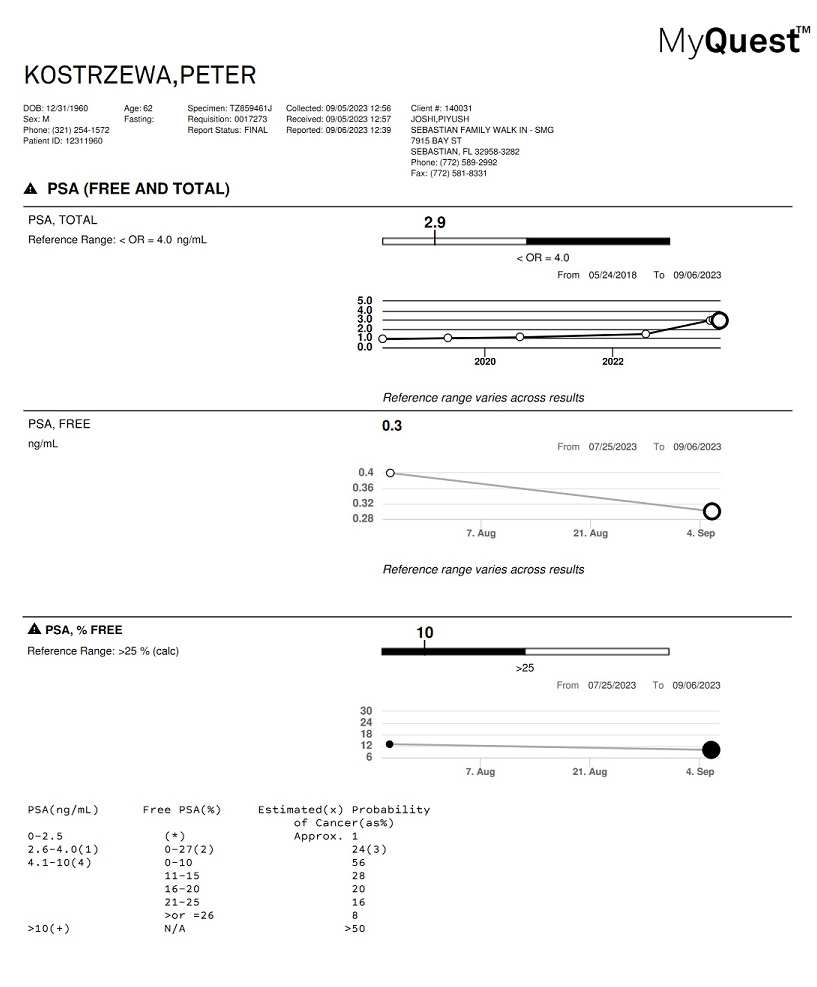
Then I noticed that my PSA—Prostate Specific Antigen, the
primary
indicator of prostate cancer—had doubled since my last report, although
it was
still showing up as green because its value (2.9) was below what is
considered
the danger zone (4). When I mentioned
this to my primary care physician, Dr, Jain (he probably would have noticed it himself if I hadn’t brought
it up),
he recommended I see a urologist—especially given our family history
where both
my brothers, my father and grandfather all had prostate cancer.
At this point, I kind of knew--or at least feared--what would happen
from talking
to my brothers and my friend Jim who had all been through this. There would be more tests to confirm that the
reading was correct. Then, it was
inevitable that I was going to have many things stuck up my butt, from
fingers
to probes to the likely inescapable biopsy tool. All
that would likely confirm the cancer,
then I would look towards treatment.
Still, despite the family history, I held out the somewhat
illogical
hope that maybe this was something else—that my situation was somehow
different.
So I met with a urologist to whom I was referred by my primary care doctor. At the first appointment we discussed general things like the existing lab work and my family history. He also gave me he expected “digital exam” (i.e. sticking his finger up my butt).
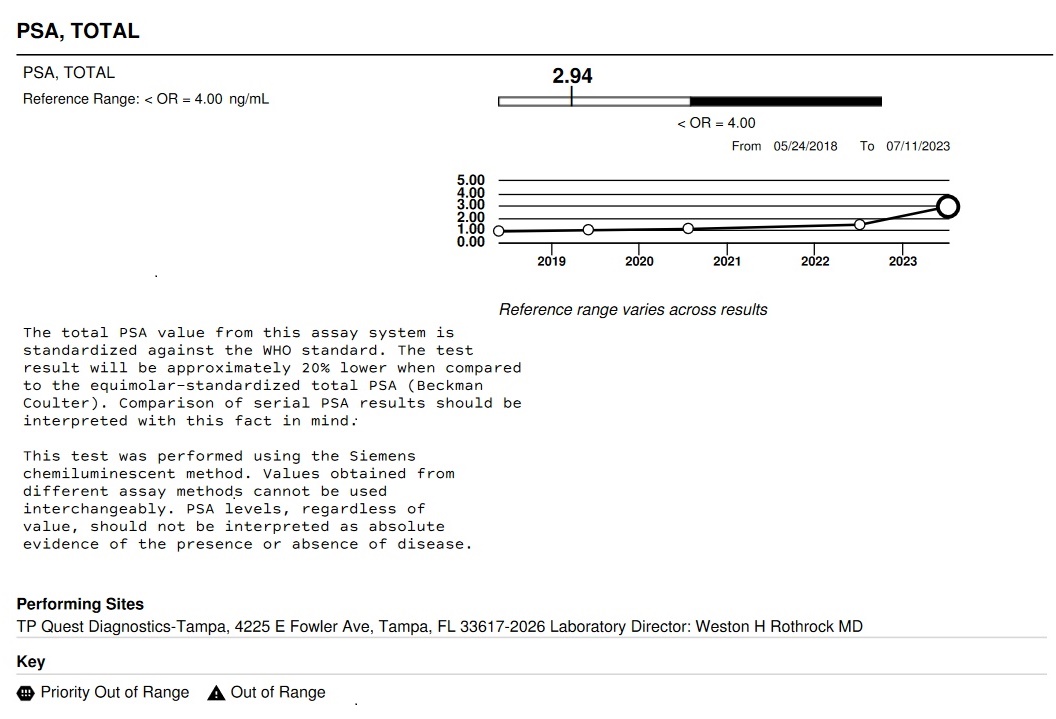
He also ordered an initial “free and total” PSA test. This test, essentially, measures the amount
of harmless and not-so harmless PSA you have and compares the two. As you might expect, you want the “bad” PSA
to le less.

At the next appointment, about a week later, they did a
urination study for which I was supposed to drink 6 to 8 glasses of water prior
to the appointment. This was my first
“full bladder” experience that would become routine much later in this
journey.
The actual test consisted of me peeing sitting down into
some high-tech toilet contraption with a blue glowing light. This analysis found my bladder was not
emptying well. In fact, I think it was
then that the doctor described my bladder as being like that of a long-haul
trucker who seldom took bathroom breaks.
This surprised me since, during my professional life and in retirement,
I’ve pretty much had the freedom to pee when I wanted. Although, admittedly, sometimes when “in the
zone” of writing code I might have foregone the bathroom for long stretches.

He also looked at the Free and Total PSA results and gave me
some behavior-modification instructions that included peeing more frequently,
even if I didn’t need to go, and, after peeing, doing it again in five
minutes. The plan was to try this for
about 6 weeks, then do another PSA test to see if there had been improvement. We also scheduled a prostate ultrasound in a
couple weeks.
At this point, I started doing quite a bit of prostate
cancer research online. I downloaded a
bunch of articles and read them. This
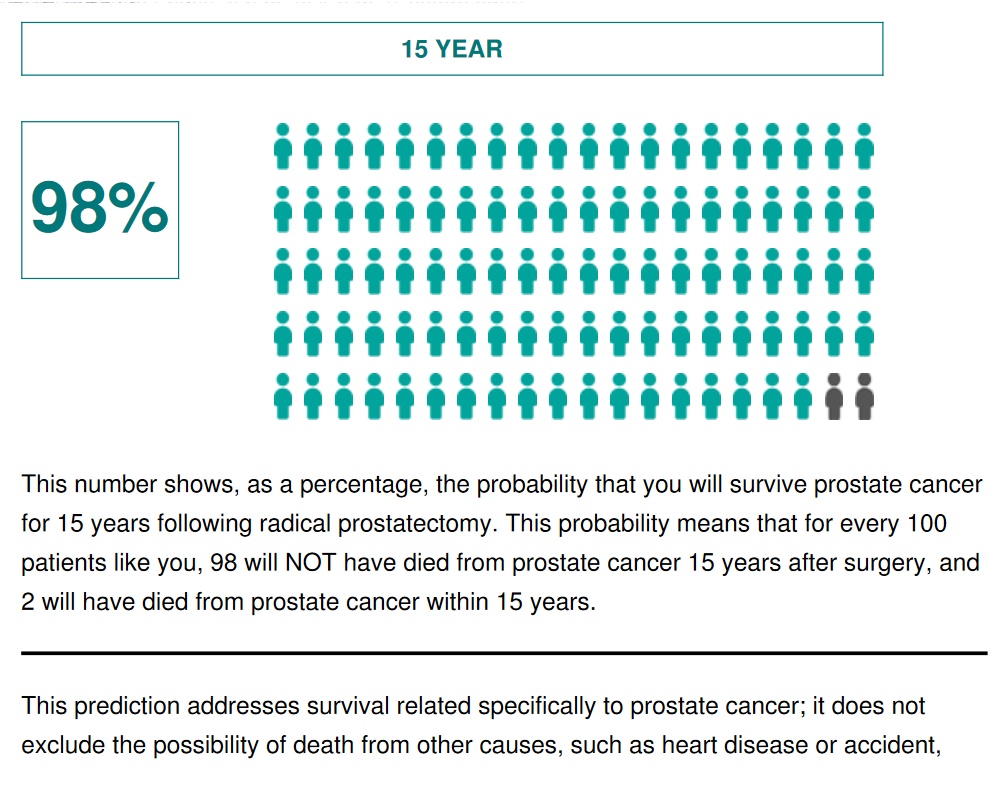
was really the beginning of my understanding of what this all meant. An article from noted cancer treatment
facility Sloan-Kettering had a chart that showed that, after removal of the
prostate (radical prostatectomy) when the disease has not spread, there is an
98% survival rate after 15 years. Sounds
good, but my thought was: “wow, there is actually a 1-in-50 this will kill
me within 15 years.” And the odds would
be worse if the cancer had already spread.
My research told me that, based on the free and total PSA
result and my age, my chances of having cancer were around 50%.
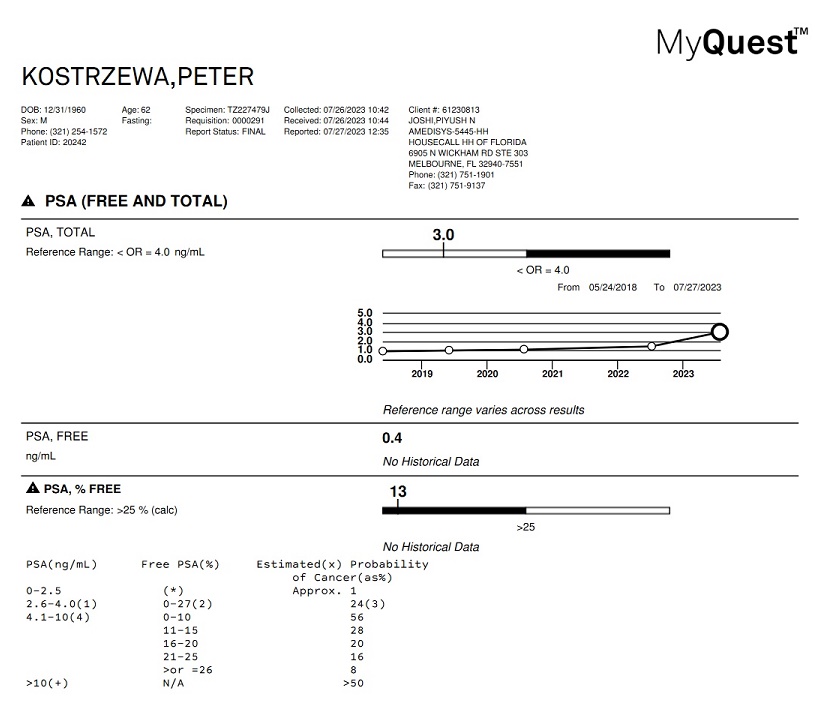

When the urologist saw the results, he put the
odds of
cancer more like 30%--actually 28% per the non-age-adjusted chart with
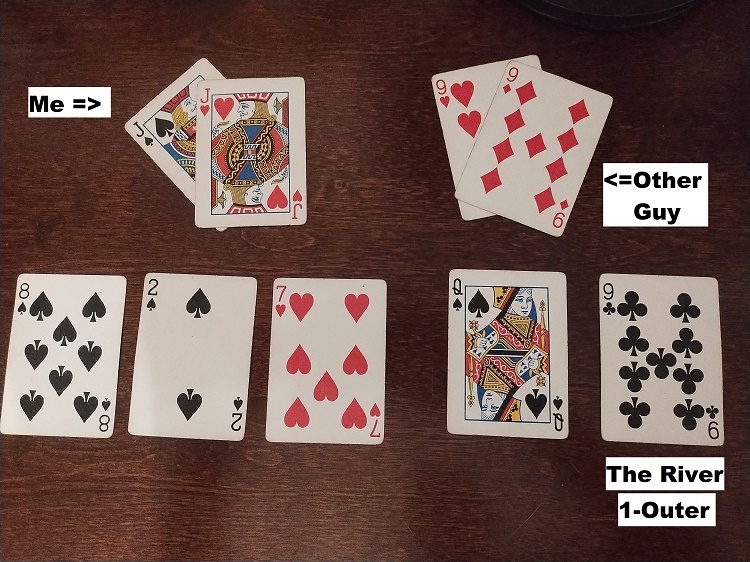
the test results. This is like me having ace-king and cancer having
ace-five
(ok, that’s more like 75-25 but close enough for government work). However, as it turns out, in the last poker
tournament I played in Vegas a few years ago, the guy who knocked me out
proudly called my ace-king all-in with ace-five and easily collected all my
chips when he got a five on the flop.

By the way, to beat the poker analogy to death (so to speak),
that 1-in-50 chance of dying within 15 years is fairly close to the odds of
losing when your opponent has exactly one card that can beat you on the river (i.e.
a “one-outer”). Ok, the odds of that are
only 44-to-1 but, again, close enough for government work. This also seems quite unlikely but it also
happened to me once in a memorable home game tournament (in poker, you tend to
remember your most unlucky hands).
The next appointment was to perform an ultrasound. This essentially meant sticking a probe with
a camera up my butt (not exactly, but close enough…) while I lay, more or less,
in the fetal position. I had to take an
antibiotic prior to the procedure, but didn’t need to fill up on water or
anything.
<Deliberately not including a graphic picture of a prostate ultrasound>
In addition to getting a better look at the prostate, this
is also meant to provide guidance for the biopsy, which is the likely next
step. I found out later through my
research that MRI-guided biopsies, rather than ultrasound-guided ones, are the
current best practice but I didn’t know enough to question the process at the
time.
The ultrasound showed that one “lobe” of my prostate (i.e.
half of it) was enlarged and pressing against my bladder, causing it not to
empty properly. While this was somewhat
of a problem, it probably wasn’t the cause of the PSA spike. In my mind, however, it was enough to provide
some hope that maybe I didn’t have cancer.
The next step would be to get the second Free and Total PSA test to see
if any improvement had occurred due to the prescribed changes to my urination
habits.
The second PSA test was done after Labor Day. Unfortunately, but not logically
unexpectedly, it showed no improvement over the first test. This meant we would be moving forward with
the biopsy, which was scheduled for about a month later, in mid-October.
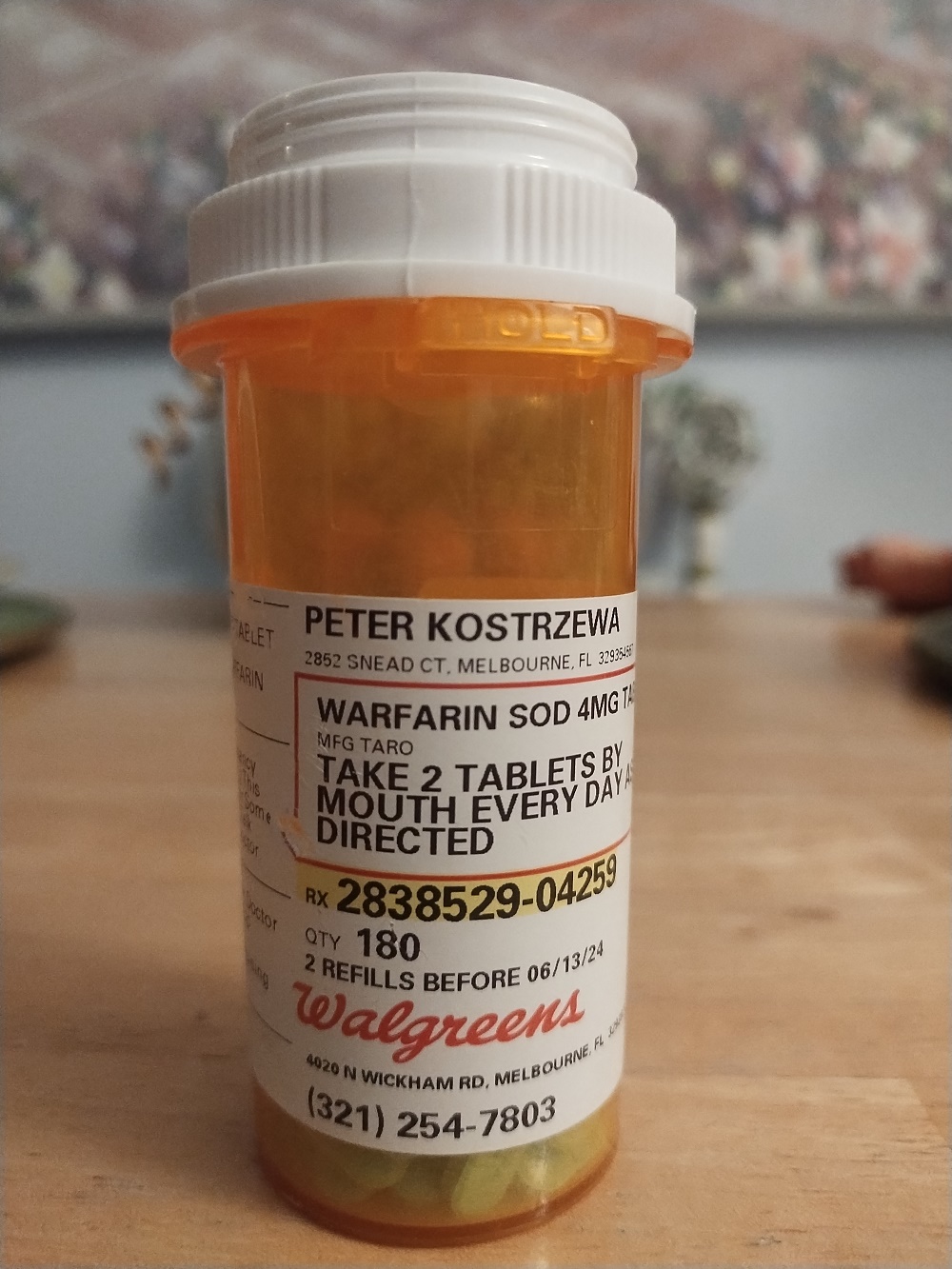
Unexpected complications developed before I could actually
get the biopsy. Prior to the biopsy, I
would need to stop taking my blood thinner, Warfarin, for a few days. To go off Warfarin, I would need approval
from my cardiologist. However, although
he tested my blood regularly and managed my Warfarin dosages, my cardiologist
refused to approve my temporarily stopping it.
He said that, since the blood thinners I was taking had been originally
prescribed after I had a mini-stroke, I’d need a neurologist to approve getting
off the Warfarin. This was a surprise to
me, as it was to every other doctor—and every logical person--that I told about
it.
At my next “Coumadin clinic” (Warfarin is a generic
equivalent of Coumadin) appointment, where, every month or so, I got my blood
checked to regulate my Warfarin dosage, I asked directly about this issue. The answer relayed to me by the nurse who
drew my blood was the same—my cardiologist would not approve my stopping
Warfarin. Another bizarre twist at the
time was my being informed that I now needed to wait in a side hallway, rather
than in the office, to get my blood test.
Maybe the blood thinner patients had been deemed not worthy of being in
the same office with serious heart patients??
This would be the last time I would ever see this cardiologist or his
hallway blood test clinic.
Now believing I somehow now needed to find a neurologist
before I could get a prostate biopsy, I called my urologist’s office to tell
them I needed to postpone the biopsy until I could get approval to stop taking
blood thinners before the procedure.
After relating the story to them, they gave me the name of a neurologist
to see. I believe I called their office
and explained my problem, but they seemed as confused as everyone else by my
cardiologist’s attitude and said they would get back to me. I don’t believe I ever heard back from them
but, as it turned out, I didn’t need to.
Coincidentally, at the same time all this was going on, I
was having these strange dizzy spells and equilibrium problems. I had had a similar problem a few years ago,
when I was still working. My doctor at
the time said it was caused by a sinus infection and prescribed an antibiotic
“Z-pack” (Azithromycin) that miraculously cleared up the problem. I was hoping this was the same kind of
problem with a similar solution, so I had made an appointment with my primary
care doctor, Dr. Jain.
While at that appointment, after Dr. Jain examined my sinuses and prescribed the antibiotic, I mentioned my problem getting cleared to stop taking Warfarin so I could get a prostate biopsy. In an amazing display of customer service, he actually called another cardiologist, Dr. Sharma, while I was in the exam room. While still in the room, Dr. Sharma’s office called me and scheduled an appointment for two days from then. His office was a ways north, in Merritt Island, but I was happy to drive the 40 minutes or so if my problem could get resolved. As it turned out, my brother Walt’s cardiologist was in the same office.

Dr. Sharma not only approved my going off Warfarin for the
biopsy, he recommended I get off of it completely and switch to a different
blood thinner—one that would not require regular blood tests. He even took the time to explain the history
of Warfarin and how it came to be used as a rat poison--the story involves
clover and dead cattle and you are welcome to Google it.
During the appointment with Dr. Sharma, we also discussed the patent foramen ovale (PFO), or hole in my heart, I apparently have had since birth. This appears to have been the cause of my transient ischemic attack (TIA), or “mini-stroke”, over 15 years prior. The TIA is the reason I have been on blood thinners all these years.
 |
 |
At the time of my TIA, a device--called an “occluder”--that
could be inserted in the heart to block the hole was considered experimental
and generally available only in Europe. I
do remember my doctor at the time explaining that, if I had a career that was
strenuous on the heart (I believe he used the example of scuba diver), I could
get the blocking device. Otherwise,
blood thinners would need to “fail”—in other words, I would need to have
another stroke—before I could be considered for the device. Not wanting to be on blood thinners, or even
confident they would work, I remember wondering if I could go to Europe to get
one of those heart-blocking devices. I
did not go to Europe but, rather, started on the blood thinners that I still
take today.
As an aside to an aside, if you remember Tedy Bruschi, one
of the Patriot legends from the early-2000s dynasty, he had a PFO like
mine. Also like me, he had a TIA, his
being in 2005 about a month after winning his third Super Bowl. Unlike me, he did get the occluder device and
played in the NFL another 3 years. I was
a little jealous at the time that he got the device, but could never really be
upset with someone who was on 3 Patriots Super Bowl teams. As an aside to an aside to an aside, Bruschi
had second, different type of stoke in 2019 but I hear he recovered well and
can still be seen on ESPN.
When I started seeing Dr. Jain in 2022, he asked why I never
had my PFO closed. I responded that I
didn’t know that was an option, since I was neither an NFL player nor a scuba
diver. Apparently, in the years since my
mini-stroke, the hole-blocking device had been approved for general use, but no
one had told me (and I never thought to look).
At the time, Dr. Jain had called a different cardiologist that performed
PFO closures and immediately set up an appointment for me. I was kind of excited with the idea of
getting off blood thinners after all these years and, after meeting the
cardiologist, was ready to go through with it.
At that time, I was still seeing the cardiologist who now
would not approve my getting off blood thinners. At a subsequent appointment
with him, I asked him about PFO closure.
He kind of implied it was a stupid idea.
Of course, he didn’t perform PFO closures.
With my two cardiologists in disagreement, I did further
research. It seems the procedure came
with risks, as any medical procedure does, but these were potentially more
serious because they involved the heart.
The device would be inserted through the groin using a tube, as might be
done for a cardiac catheterization. Both
my father and Pat had had those and survived quite well so that really wasn’t
something I was worried about. More
telling was that the procedure was seldom done on people my age, therefore,
there was little data on the success rate and complications on people in their
60s. My indecision became moot when I
realized the hospital where the procedure would be done was not in my insurance
plan and I certainly wasn’t prepared to pay for a heart procedure out of
pocket. So the idea of closing the hole
in my heart was shelved.
Now, almost a couple years later, I was meeting with a third
cardiologist who also performed PFO closures.
I was excited about getting a tiebreaking opinion on the issue. The debate was resolved when Dr. Sharma said
that, after evaluating my situation, he would not recommend my getting the
procedure. I was happy that that case
was closed.

So, as it turned out, needing a prostate biopsy indirectly resulted
in my no longer needing monthly finger stick appointments to regulate my
Warfarin, no longer worrying about whether I should get the hole in my heart
closed and got my approval to stop blood thinners long enough to get the
prostate biopsy. Plus, I got to learn
about the history of Warfarin and significantly upgrade in my cardiologist, who
I met with in an office rather than a hallway.
After finally getting the approval from a cardiologist, I
rescheduled the biopsy for the first of November. This particular urologist did a couple things
that I didn’t expect, based on discussions with my brothers and my friend Jim who
had had biopsies previously. First, he
had me do an enema before the procedure.
My research showed that some urologists would request that, although it
seemed this was more common in other parts around the world. So that was a new experience which I will not
describe and which no one wants to hear about.
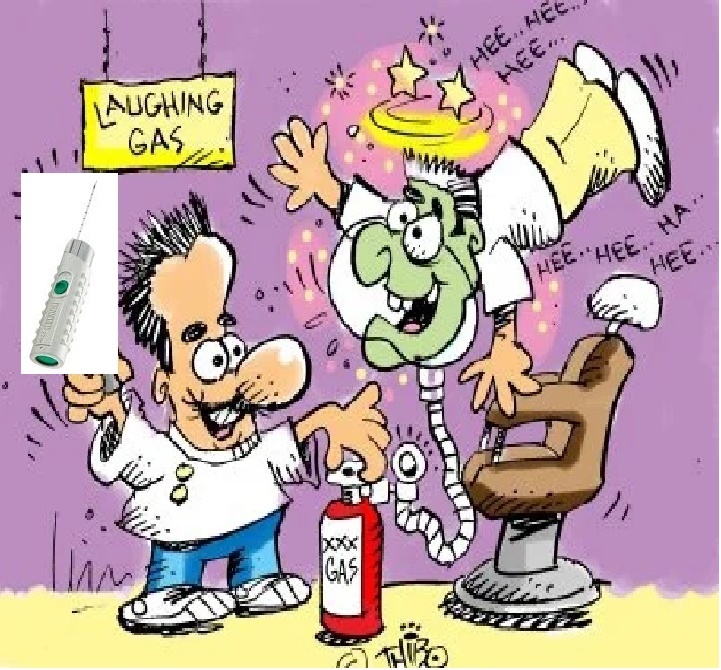
The other unique thing this urologist offered was to provide
nitrous gas to kind of distract you from the pain during the biopsy. Apparently, outright sedation does not work
in this type of procedure, maybe because you need to be somewhat awake? Using a gas that dentists used to use (maybe
they still do?) during a biopsy was something I could find no evidence of being
done by anyone else. Further, insurance
would not cover nitrous, so it would mean paying $350 out of pocket. In the end, I decided to do it, partially
because it sounded intriguing and maybe also because of the “hard sell” by the
office manager, who I believe was the doctor’s wife. When scheduling the biopsy appointment, she
did the old salesman trick of saying something like: “and you’re having he
nitrous, right?”
The day of the appointment, Pat had come with me to drive me
home as I would be taking some prescribed Valium before the procedure. After doing my enema (which I still won’t
describe) and taking pre-procedure antibiotics, we were on our way. When we got there, it was clear they were
running well behind. The waiting area
was full of angry old men with various urinary issues who would intermittently
go to the front desk to ask how much longer it would be. When I checked in, they asked if I had
brought my Valium to take before the biopsy and, ever the good patient, I
proudly showed them the bottle I had brought.
Problem was, I had somehow brought the leftover antibiotics from the
ultrasound rather than the Valium. Here,
the fact that they were running so late worked to my advantage as I had time to
make the half hour round trip home to get the correct pills and return well
before they were ready for me. So my
pill mix-up only meant I had a half-hour less of reading stuff on my phone
while waiting.
When I was called, I went in and took my Valium. After changing into the dreaded gown and
entering the procedure room, it was time for the nitrous, which was very
interesting.
While I’m lying there, again in the fetal position with
something stuck up my butt, the gas was flowing through the gas mask. I was immediately in a euphoric state. In fact, my senses were transported to many
years ago when my friends and I used to routinely get very drunk. I had the taste of many beers in my mouth and
the musty, dank smells of a busy dive-ish bar—the bar might have been the Cask
and Flagon, near Fenway in Boston. Thoughts
of my best friend back then, with whom I had experienced countless severely
drunken experiences, drifted into my mind.
With a feeling of severe impairment, it probably made sense that my mind
went back to a time of my life when that state was a regular weekend occurrence. It might be worth noting, however, that, in
this moment, the best friend I thought of years later realized (or accepted)
that he was gay. You can choose to add
whatever Freudian implications you want about this situation where I had this
giant thing stuck up my butt and thought about time I spent with a gay man.
In any case, the nitrous certainly did its
job. Despite the fact that I was awake
and could clearly hear the doctor’s voice and the loud click of the biopsy
tool—which sounded like a staple gun—I just felt euphoric.
 |
 |
Prostate biopsy under nitrous (not
an actual picture of the biopsy, although this does look like my
urologist, cartoon from juliahailes.com)
|
Under the influence of nitrous, I imagined I was as THe Cask outside Fenway in the 1980s
|
One thing I clearly remembered was that, after one of the
clicks of the biopsy gun, the doctor said something like: “I’m doing another
one.” In my mind I figured he either
“mis-clicked” in one spot or saw something he didn’t like. I tried to keep count of the staple-gun
clicks, knowing he was supposed to do 12 of them. I’m not superstitious but I was pretty sure I
counted an unlucky 13 shots.

After the biopsy was over and they were going to flush the
nitrous out of my system with oxygen, I almost told them not to. I was thoroughly enjoying the experience. But flush they did and, in a flash, I was
sober and back in the present. Shortly thereafter,
Pat was driving me home and all there was to do was to wait for the results.
Me and my sore and sometimes bleeding butt had to wait a
couple weeks for the appointment to get the biopsy results. I wouldn’t say I was anxious about the
results but, for some reason, I began to believe that the results would be
negative and I would be able to go on my way.
The day of the biopsy results, the office was again very
busy and appointments were running well behind.
And, as is typical with doctor visits, my name being called only meant
that I got to wait in a different, private room for a while longer.
When the doctor finally came in, he told me I had
cancer--the hope that it was some other benign condition was gone. He described the cancer as “borderline bad
boy cancer” which didn’t sound like a very technical definition. I had a lot of questions, but he was clearly
in a hurry and told me he would loan me a book that I could read. He did mention that freezing the prostate was
an alternative to surgery and that sounded interesting. However, my later research informed me that
this isn’t really an option that is used, except in rare cases, making me
wonder why he would even mention it.
In the end, the doctor said he would refer me to a surgeon
in Orlando. The surgeon turned out to be
the same one who had operated on my friend Jim and my brother Walt. From their experiences I knew this was a
world-renowned prostate surgeon to whom people came from all over the world to
see.
Still, it felt like things were moving very fast. As I was checking out and paying my co-pay, I
asked about getting an MRI and/or CAT scan which my limited research at this
point told me I should have. The doctor
and his assistant only said
that the surgeon would ask for whatever scans were needed. And they told me to read the book. They did schedule blood work and a follow-up
visit for February and March, assuming the surgery would be long done by
then. Again, this seemed very quick,
given that this was mid-November. I
definitely did not leave the office feeling confident.
So now I definitely had cancer. The next step was figuring out what I wanted
to do about it.
| Home |
Previous |
Next |