Shortly after my diagnosis, I made the decision to let all
my relatives know about it. I had,
admittedly, done a pretty poor job of keeping in touch with everyone over the
years. We might see each other for
dinner when we were visiting New England or maybe exchange an email here and
there, but not much else.
When my Auntie Nina passed away at 100 years old in 2020,
that meant all our relatives from that generation were gone. Years earlier, we had lost my cousins Lee and
Joyce. Our family shrunk more when Joyce’s
son Michael, my second cousin, succumbed to brain cancer in 2023, followed by
my godmother and cousin Barbara dying of kidney disease the next February. I didn’t like the fact that I was mostly
seeing my cousins at funerals, so I saw my diagnosis as a potential way to
start regularly communicating with them—before we lost anyone else.
I figured it was easiest to just create an email list containing
all the cousins I had addresses for and send a message explaining my
situation. I got such positive responses
from them that I kept sending periodic updates.
These exchanges ultimately led to in-person visits, resulting in my
feeling closer to my cousins than I had in years. This was definitely a positive that came out
of what could have been very negative circumstances.
My urologist’s office had said they would send all my
information to AdventHealth in Orlando and they would soon contact me to set up
an appointment. While waiting for that
call, I started reading the book the urologist had loaned me. I quickly finished it and learned many things
but, overall, I found it lacking. First,
it was about 6 years old, so I knew it did not have the latest
information. Second—although I don’t
think I’m biased against female doctors—I wondered, at least subconsciously,
why a woman was writing about something that is exclusively a man’s problem. So maybe I was biased against the book to
start.
Towards the end of the book when side effects—especially
worst case ones—were discussed, there was a line that said something to the
effect that: if you can’t have sex anymore you can still hold hands. I’m sure the author was just trying to say
that, if the side effects were bad, it still wasn’t the end of the world, but
the sentiment somehow felt condescending.
During this waiting period I also spoke to both my brothers and my friend, Jim, about their experiences with prostate cancer. All of them had opted for surgery. I got copies of the data they had received from their biopsies and subsequent appointments. I read through their biopsy reports which detailed things such as how many of the 12 samples, or “cores,” from the biopsy contained cancer as well as the severity, or Gleason score, and size of each cancer occurrence found. I believe I also looked at an MRI report that my brother Walt had. At this point, I had none of this data. All I had was my urologist’s verbal declaration that I had “borderline bad boy cancer.”
Unsatisfied with the information from the loaned
book, I
sought out something better from—where else—Amazon.
I found what I was looking for in “Dr.
Patrick Walsh’s Guide to Surviving Prostate Cancer,” a current-year
update to a
book by the pre-eminent prostate cancer doctor, Patrick Walsh. Note that the book was updated by a woman,
Janet Farrar Worthington, so I guess I had gotten over whatever bias I
might
have had against female prostate cancer experts.
While continuing to wait for the call from the
surgeon’s
office, I dissected the book, making notes and jotting down tons of
questions. All the information, in my
mind, confirmed my belief that things were moving a little fast.
First, a second reading of the biopsy should be
done before
anything. Apparently, interpreting the
images from the biopsy and assigning a numeric score to each cancer
requires
some level of judgement by the person reading the biopsy.
Because there is subjectiveness in this
effort and human beings sometimes make errors, a second person should
review
the biopsy.
Second, I found that modern best practice would
have been to
perform an MRI prior to the biopsy, rather than just an ultrasound as
my
urologist had done.
I also discovered there are new scanning
technologies that
can better define and characterize the cancer.
There is even a special scan—a PSMA-PET scan—that can
essentially detect
prostate cancer anywhere in the body where it might exist and thus
definitively
determine if the cancer has spread.
There are also genetic tests that can further define elements
such as
the likely aggressiveness of the cancer.
None of this information was in the older book.
The Walsh book also had much more current detail
about the
three basic prostate cancer treatment options: surgery, radiation and
hormone
therapy. In cases where the cancer is
not aggressive, there is also an option to, essentially, do nothing and
monitor
the cancer to see if it is growing to the extent that treatment is
necessary.
I was somewhat familiar with hormone therapy from
my
father’s experience with it over 20 years ago.
He chose this option because he was in his 80s when he was
diagnosed and
had other health problems, making surgery or radiation unwise,
impossible or
unnecessary (i.e. he would likely die of something else before the
prostate
cancer got him). Back then, I believe
estrogen was the typical hormone treatment and it resulted in expected
side
effects such as hot flashes.
A side effect less mentioned was that the hormone
treatment
also weakened his bones, resulting in terrible osteoporosis. Because of his weakened bone structure,
several of his vertebrae fractured over the years and became a source
of
constant pain for him.
The “solution” to the osteoporosis was infusions
of Zometa,
a drug produced by Swiss pharma giant Novartis that is often used to
treat bone
cancer. These treatments had the
unexpected—and unadvertised--side effect of bisphosphonate-related
osteonecrosis of the jaw (BRONJ), or jaw necrosis.
Essentially his teeth and parts of his jaw
started rotting and falling out. We only
found out the cause of this from his dentist, who had heard about this
Zometa
side effect. In fact, he had other
patients with the same problems.
When my parents told the doctor delivering the
Zometa to my
father what the dentist had said, the doctor apparently said something
like the
Zometa was doing more good than harm.
So, being folks that believed in taking the advice of “smart”
doctors,
my ma and dad decided he should continue the treatment.
Eventually, my father’s teeth got much worse,
making it
difficult for him to eat. The doctor
finally agreed that the Zometa should be stopped, but the damage had
already been
done.
At some point, dad was so upset about his teeth
falling out
that he asked me if he could sue anyone over his situation. Consulting Mr. Google, I quickly found that
there WAS a multi-jurisdictional lawsuit on this exact side effect of
Zometa. So I contacted the law firm
handling
the case and they were very excited to take dad on as a contingency
client—we
would pay nothing and they would get 40% of whatever settlement was
received. I remember the person to whom I
spoke saying
that dad’s case was solid, with all sorts of documentation of the
problem. He said the lawsuit was “in the
red zone” (the
football red zone, not like a warning on a tachometer) and that the
expected
average settlement would be north of a million dollars.
Apparently, Novartis decided to fight the case
rather than
settle, so it wasn’t in the “red zone” as much as we were led to
believe. The fact that this case was not
certified as
a class action suit meant that there would be trials for each
individual
plaintiff until there was a settlement or until the folks suing died
and/or gave
up. The case dragged on for years and
results in the courts were mixed with some wins and some losses.
 |
 |
Every now and then, dad would receive information or
inquiries in the mail regarding the case.
He was living by himself and close to 90 years old by now. Talking with him on the phone one night, he
told me he had received a questionnaire about the lawsuit in the mail. I urged him to wait for my next visit so I
could look it over, but he insisted on filling it out and returning it on his
own, even though he really didn’t understand all the questions. As it turned out, the questionnaire was from
the defense attorneys. Sometime later,
he actually had to be depositioned and the defense attorney was relentless in
making him sound foolish due to his questionnaire answers. I was allowed to listen in on the deposition,
but not say anything, which was very frustrating.
From the defense attorney’s questions, I could
tell dad’s
case was going to be doomed by the fact that he had found out what the
drug was
doing to him (from his dentist) but continued the treatments. Apparently, the lawsuit was also filed too
long after he stopped treatment. Ultimately,
dad died before the case was resolved and, although we were given the
option to
continue, we just dropped it.
As it turns out, in addition to selling dangerous
drugs
without warnings, Novartis was busy with flat out fraud as well. In 2020 Novartis paid a $642 million
settlement for bribing doctors and patients to use their drugs (you can
read
about it here). If you wonder
why Medicare
is becoming insolvent, at least part of the reason is corrupt companies
like
Novartis who are ripping them off for hundreds of millions of
dollars—I’m sure
they’re not the only ones.
But I digress.
Although the lawsuit was not a positive
experience, I did
learn some things. One was that I saw
first-hand how relentless Big Pharma lawyers can be.
The guy who questioned dad had no problem
humiliating an old man and he probably got a bonus when my father died
and our
case was dropped.
Another thing I learned is that you cannot just
take
information or advice provided by doctors or drug companies on faith. When you have a medical condition, you really
need to do research and “become your own advocate.”
As a side note to a side note to a side note, many
years
later I saw an interesting episode of one of my all-time favorite TV
shows, “American
Greed.” It was about a scamming
attorney
who won big settlements for clients who never saw the money. He embezzled it from them to fund his lavish
lifestyle. The law firm was Girardi and
Keyes—the ones who handled my father’s case.
So maybe it was good to know that we never really missed out on
that
million dollar settlement as the money would have gone to fund
Girardi’s
yachts, luxury homes and cars.
 |
 |
All of dad’s medical problems in his latter
years—hot
flashes, osteoporosis, cracked vertebrae and rotting jaw and teeth—all
stemmed
from his taking hormone therapy for prostate cancer.
My brothers and I have wondered whether dad
might have had a better quality of life if he had done nothing about
his
prostate cancer. Perhaps, with the way
prostate cancer is thought of today, that might have been the
recommended
option.
So that was a series of major digressions and
rants to
explain my going-in concerns about hormone treatments for prostate
cancer, as
well as why I might want to do my own research rather than blindly
accept the advice
of the first doctor with whom I talked.
As it turns out, hormone therapy alone is really
only used
as a primary treatment for people in really bad shape who have no real
hope of
being cured or for older patients, like my father, whose age and other
health
conditions make surgery or radiation impractical and difficult to
impossible. So, hormone therapy alone
would not be an
option to treat my cancer.
At this point I realized I had two viable
treatment options:
radical prostatectomy—surgical removal of the prostate—or radiation
therapy. I found that, although surgery
had long been considered the “gold standard” of prostate cancer
treatment, a somewhat
recent study found that radiation therapy was just as effective as a
cure. The fact that radiation is an option
that is
as curative as surgery seemed unknown by most, including my primary
care
doctor. Most thought radiation was only
used in older patients who might not have a long life ahead of them.
While I was reading and digesting the information
in the
book, I realized I needed my records from my urologist to determine how
severe
my cancer was and what my actual options were.
I also realized it had been a week and I hadn’t heard from the
surgeon’s
office yet so I gave them a call. The
person I talked to assured me that, if I had been referred, I would be
getting
a call soon. After another week went by,
Thanksgiving had passed and I decided to call them again.
They said they had no record of a referral
for me, but would send me an 11-page application to fill out if I was
interested in becoming a patient. They
also said I needed to get my records from my urologist and send them
with my
patient application form. I wondered why
my urologist’s office had not done all this already.
So I started filling in all the historical medical
information and family history that the form requested.
I remember being annoyed that, rather than an
electronic form, they sent you one you had to print out, fill in by
hand, and
scan back in. While I was working on the
form, I called my urologist’s office to ask about getting my records
but, for
some reason, I couldn’t reach them—no one answered and no voice mail. I decided to drive by the office, figuring I
could return the book the doctor had had loaned me while getting a copy
of my
records. This attempt also failed as I
found the office closed on a Wednesday afternoon, making be wonder if
they were
still in business.

Eventually I found the office open and explained that the surgeon didn’t have my records, plus I wanted a copy of them for myself. They told me they couldn’t just print out my records and hand them to me. They needed to be signed by the doctor, or something, and date-stamped. That seemed ridiculous as they were my records and I (and my insurance company) had paid for them, but I wasn’t going to create an incident over it so I waited some more.
While there, I also asked about sending my biopsy
results off
for a second reading, which all the books recommend.
They just said, of course, that the surgeon
would handle that. It seemed pretty
clear that they had already “handed me off” as a patient.
About a week or so later, the office called to say
my
records were ready. I zipped down there
to pick them up. When I did, they
assured me that, this time, they were being sent to AdventHealth.
By the time the records were ready, I had already pretty
much finished reading the second book and was anxious to get my data so I could
characterize the cancer more definitively than “borderline bad boy
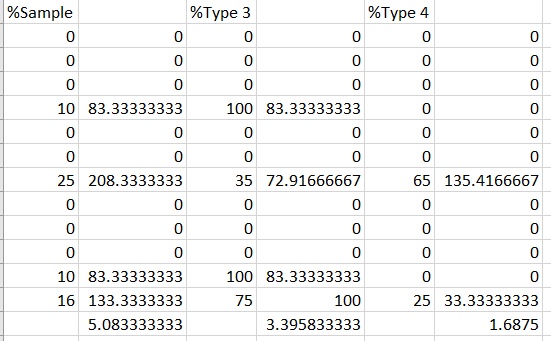
cancer.” I had learned that the key
number was the Gleason score, a measurement of how organized, or aggressive,
the cancer is. A score of 1 or 2 means
no cancer (and aren’t actually used anymore), 3 is not so bad, 4 quite a bit
worse and 5 the worst. The actual
Gleason score is a sum of the 2 most dominant types of cancer in each positive
sample so, if a sample is, say, 25% 4 and 10% 3, the score for that sample is 4
+ 3 = 7. So the overall Gleason scores
run from 6 to 10 but, within the scores there are differences with, for
example, a 4 + 3 worse than a 3 + 4 because the 4 + 3 has more aggressive
cancer. The overall Gleason score is simply the highest score of all positive
samples.
To better summarize prostate cancer, they
eventually came up
with a grading system that assigns a 1 to 5 score (5 being worst) based
on the
Gleason scores. The grade also makes it
much easier to explain to people how bad the cancer is.
Examining my records, I found that 4 of my 12
biopsy samples
had cancer with the grades being 1, 1, 2 and 3 for an overall grade of
3 of
5. The other information in the biopsy
included the size of each cancer, the size of the prostate and whether
there
was evidence of cancer escaping the prostate (there was not, which was
good).
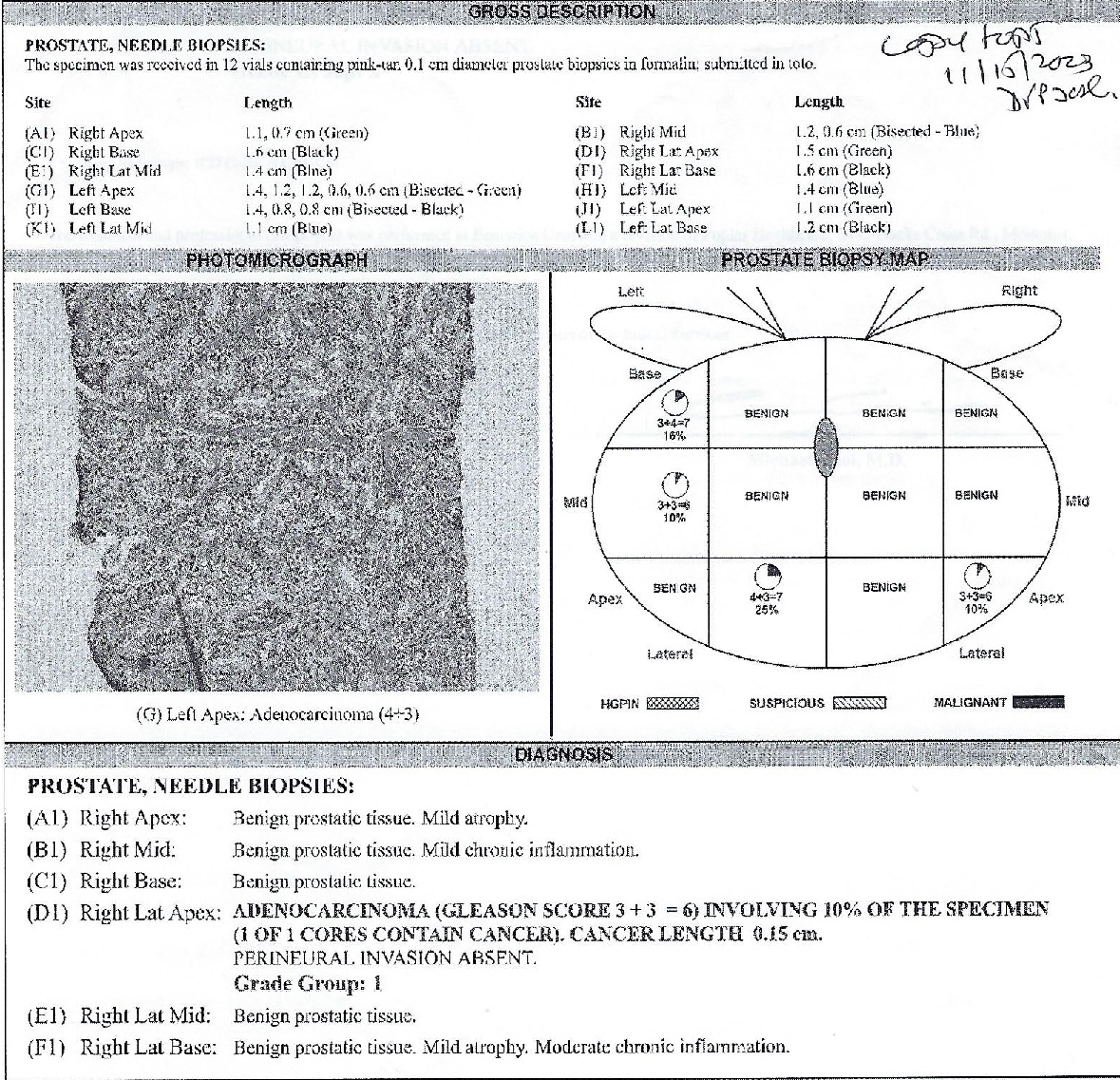
I parsed the data every way I could, including
creating a
spreadsheet to calculate the percentage of my prostate that had
different
cancer types. Turned out, by my
calculations, only about 3 ½ percent of my prostate had cancer and only
a
little over 1 ½ percent was the bad one—so how hard could it be to
treat that
relatively small amount, I thought.
Turns out there is also a “stage” for prostate
cancer, but
it seems less relevant than the grade. I
calculated my stage to be T1c, meaning the tumor could not be felt via
a rectal
exam and had not metastasized (spread).
That sounded good, too.
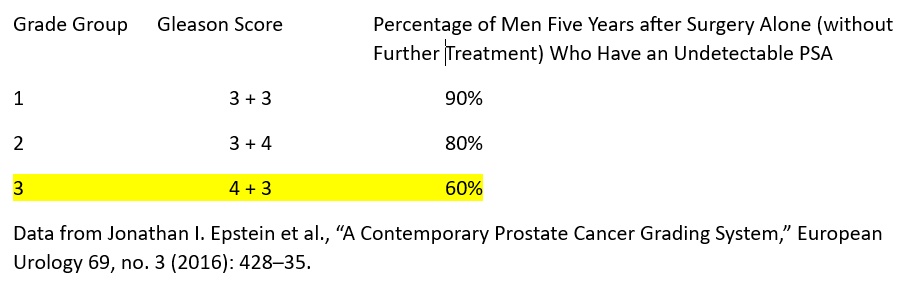
More sobering was a chart I found in the book that
showed
that, with grade 3 prostate cancer, 5 years after prostate removal,
only 60% of
patients had undetectable PSA. In other
words, the cancer came back within 5 years for 40% of men with grade 3
cancer—my grade. And with my luck, that 40% felt like 99%.
By the way, in case there weren’t enough numerical
ways to
characterize prostate cancer, there is also a verbal description. Mine was the rather ominous-sounding
“unfavorable
intermediate.”
So now I knew more about my cancer.
The first takeaway was that it could not be
ignored, so the “watchful waiting” option was out.
From all my reading, I knew there were two
ways to cure it: surgery or radiation, although I still needed to talk
to a
specialist to know if radiation was truly a viable option.
By now, I had created pages of notes from my
reading and had lots of questions about potential treatments.
From my brothers and my friend Jim I already knew
surgeons
pretty much no longer do the cutting directly when performing ordinary
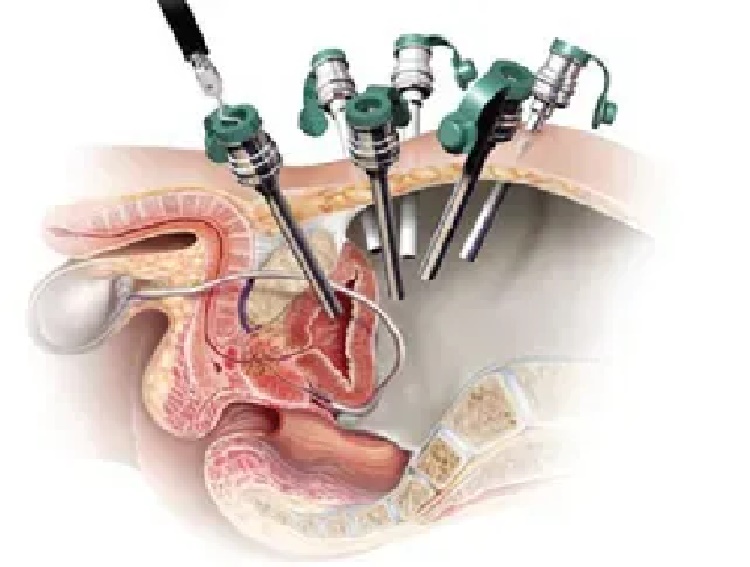
prostatectomies. Instead, a robotic
device, called a Da Vinci, is operated remotely by a surgeon. The surgical tools are inserted through small
holes cut into the abdomen. In my mind,
I envisioned the surgeon looking like he’s playing a video game or
maybe using
one of those arcade crane games where you try to grab a good prize.
 |
 |
The book was very helpful and gave me an
appreciation of
what my brothers and friend Jim had gone through. However,
several times while reading it I had
to stop and put it down. The passages
describing the details of the surgery were just too upsetting for me to
get
through. I believe both my doctor and
the book referred to URLs where you could watch videos of actual
prostatectomy
surgeries. Who the heck would want to
see that?? Probably a lot of people, I
guess, but certainly not me.
The other difficult thing for me while educating
myself was
the realization that there were no great options to cure prostate
cancer. Each approach had unavoidable
risks and
unavoidable side effects. With surgery,
you have to worry about blood clots, infections and hernias, as well as
the
risks all surgeries bring. With
radiation, there is the risk of the radiation damaging adjacent areas,
especially the rectum. Radiation also
could bring fatigue and urinary frequency.
Both options bring long term potential urinary incontinence and
impotence. Further, given my grade of
cancer, with radiation I likely was looking at temporary androgen
deprivation
therapy (ADT), aka hormone treatment, with (hopefully temporary) side
effects
such as hot flashes, more fatigue, weight gain and loss of muscle mass. I realized that, going forward, my life would
be different—some things would not be as “good” as they were in that
moment, no
matter what option I chose.
I guess, in my mind, I was always somewhat biased
against
the surgery option. I think, given a
choice,
most people would avoid surgery—or at least delay it as long as
feasible. Although surgeries are very
routine and
millions are probably performed every day, there are still inherent
risks.
Years ago, early one evening, I got a call at work
from
Pat. One of her best friend's husband
had been in the hospital for knee surgery, but there had been
complications
with the anesthesia and he was in grave danger.
She asked me to come to the hospital for support.
Initially, I said no as this was not long
after my mother, Pat’s mother and several other family members had died
and
I just didn’t want to go to another hospital.
Ultimately, I did go, however.
It was after visiting hours and I had to use a
back entrance
and walk a long way to the room. When I
finally got there, I saw the husband lying motionless on the bed. However, every 30 seconds or so, his body
would convulse and his eyes popped wide open.
They said he was brain dead and they were waiting for his sons
to get
there so they could see him before they removed him from life support. My job wound up being to go pick up one of
the sons that was flying in. I was
certainly relieved when I was able to leave the room.
That image of a man convulsing in a hospital
bed after he had come in for simple knee surgery certainly was burned
into my brain
since then. That memory likely
contributed to my anti-surgery prejudices.
The prostate is connected to the bladder and the
penis—two
pretty important things. Radical
prostatectomy removes the prostate, then stitches everything back
together with
the hope that everything still works afterward.
The surgery has become routine and is performed thousands of
times a day
but I still worried, somewhat, that mine would be the one where the
surgeon
made one slip-up and I would be peeing in a bag the rest of my life. Or maybe the hole in my heart and irregular
heart
rhythms would lead to some complication.
Or maybe there’s a problem with anesthesia, as I witnessed years
ago. These types of outcomes are, of
course, extremely rare and these fears are probably not rational, but
they were
still in my mind.
Logically, I’d go in for surgery, they’d do it,
I’d stay in
a hospital for a day or two, and I’d go home with a catheter which
would be
removed a few days later. After that
there would be healing for some time and regular blood work, but,
essentially,
I’d be “done” with treatment after a week or two.
Further, after the prostate is removed, it is
actually
dissected it to determine if the cancer existed on the borders of the
prostate. If that were the case, the
surgeon could go back in and remove more tissue, hopefully keeping the
cancer
from spreading.
Being “done” that quickly assumes that follow-up
bloodwork would
show my PSA remaining at zero which, according to the table cited
above, won’t
happen 40% of the time. In those
situations—as was the case with my brother Walt-radiation would be in
order
but, for the majority of patients, the big stuff is done in a week or
two.
Radiation would be a much longer time commitment. There would be many steps to prepare for
radiation, then daily treatments for several weeks.
After treatment, PSA would need to be
monitored for years to make sure the radiation was effective. If the PSA does start rising too fast, the
whole process, including radiation, would likely need to be repeated. It is unlikely surgery could be performed
after radiation because of the damage the prostate would have incurred
from the
radiation. For these reasons, most men
choose to just “cut the cancer out of me” and be done with it as my
brothers
and Jim had done.
With my records and patient application forms sent
to the
surgeon’s office, I finally got a call to schedule my appointment at
AdventHealth. It would be at the end of
January—over 2 and a half months after my initial diagnosis. By the time of my appointment, I felt really
ready, armed with my pages of notes and all the questions I had
highlighted. The research I failed to do
was finding out what the AdventHealth facility actually did. Because the information package I had
received said I would be meeting with a “team” of experts, I had
assumed I
would be able to ask about all the options for treatment and get all my
questions answered. In actuality, this
facility only does surgery, which I would have known if I had done a
bit more
homework.
The day of my appointment finally came and I took
the hour-plus
drive to Celebration—the Disney-created community outside Orlando. Speaking of Disney, even though I was
following my Google directions, I still managed to make a turn too
early and
found myself in the parking lot of Disney’s corporate offices. Luckily, Disney security did not detain me as
a potential corporate spy and I was able to exit their lot, do some
backtracking,
make a likely ill-advised U-turn and arrive at Advent early for my
appointment.

After depositing my car in the first garage I
found, I looked
at the provided map and started trying to figure out where the building
I was
supposed to go to was in the somewhat sprawling campus.
When walking out of the garage, a young woman
with crutches who might have been a cancer patient asked me for
directions. I explained this was my
first time there, but we ultimately both found the cancer buildings we
were
going to. This was the first time I
actually thought of myself as a cancer patient.
The day started with yet more paperwork, a check
of my vitals
and providing a urine sample before moving to the substance of the
appointment. Over the next couple hours,
I met with several nurses and/or assistants who provided various
information
about prostate cancer and the surgery, a lot of which I had read in the
book. It was somewhere in this process
that I realized this was all going to be about surgery.
I asked the final nurse with whom I met what
I would do if I wanted to consider other options, like radiation. Were there radiation specialists at Advent
that I could talk to? She
said they had no radiation doctors there
but that I could ask the surgeon about it when I talked to him. In retrospect, seems like that would be like
going into a McDonald’s and asking for directions to the nearest Burger
King.
One of the women with whom I met talked to me about getting a genetic test. I was happy to hear this, as I had read how genetic tests could be useful in predicting how aggressive the cancer might be, identifying mutations that could lead to future cancers and possibly warning if other relatives (in my case, my nephews) could be genetically predisposed to prostate and other cancer. I had actually planned on asking if I could get a genetic test done.
They had me fill out an online application for the genetic
test on my phone. That process was a
little dicey as I had a crappy, old phone.
After I was nearly done, something went wrong and I had to re-enter all
the info again. In the end, the
application came back and said, based on my insurance and income level, the
test would cost less than a hundred dollars, which was fine with me.
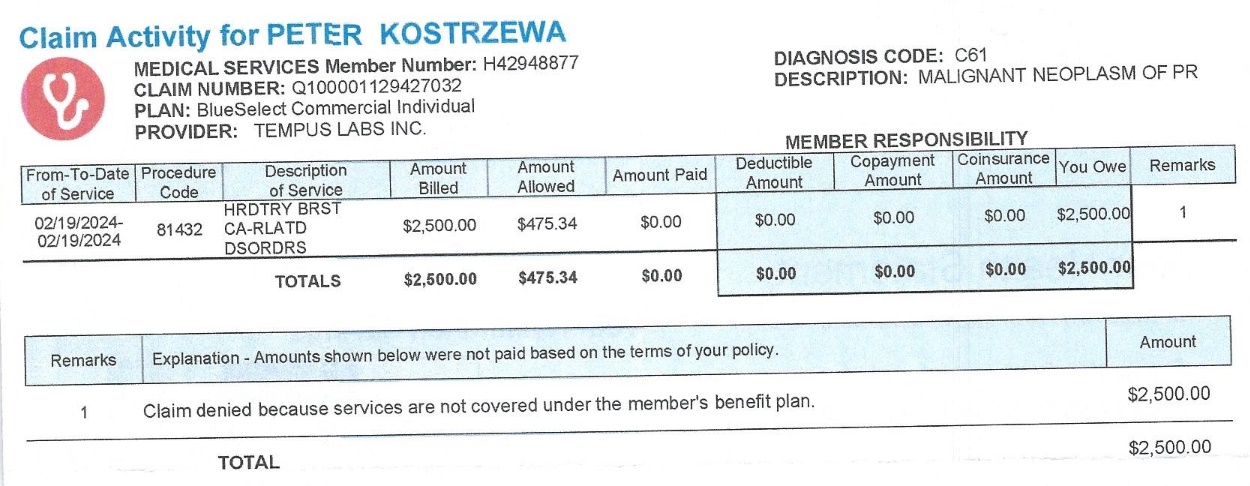
As a sidenote, months later I got an Explanation
of Benefits
from Florida Blue that said the claim for the test had been rejected
and I
could be billed $2500. Around the same
time, I got a letter from the genetic test company with a form to fill
out and
sign authorizing them to appeal the rejection.
I haven’t heard back from anyone asking for the $2500 so maybe
the
appeal was successful. Either way, no
one’s getting $2500 from me for the advertised $100 test.
So, with the application approved, the nurse in
charge then
said she would draw a blood sample for the test. I
was thinking this was really efficient as
everything would be done right then and there. I
was mistaken. The nurse was unable to
complete the blood
draw. It was pretty obvious she hadn’t
done it a lot, as she was muttering instructions to herself. After her failed attempt, she said she would
get another nurse who was an expert at doing blood draws.
The second nurse also failed. All
this surprised me because, whenever I’ve
had blood work, the phlebotomists generally had no problems and some
said I had
great veins.
In total, three different nurses attempted to do
this simple
blood draw and all of them failed.
Finally, they gave up and said they would send someone to my
house to
get the blood sample. I have to say,
this was quite disconcerting. Here were
the nurses that would presumably be assisting with this quite serious
surgery I
was considering but they couldn’t perform a very elementary task. By the way, the nurse they sent to my house
to draw the sample had no problem and, I believe either laughed a bit
or was
incredulous when I told her three nurses failed to complete the draw at
the
office.

Among the questions I asked one of the nurses was
whether I
could get scans using the latest technology I had read about. Specifically, I had read about a
multiparametric MRI that would provide 3D images and, more importantly,
the
PSMA-PET scan, which is designed to specifically detect prostate cancer
anywhere in the body. I felt this would
be hugely significant if I could get one because it could tell if the
cancer
had spread anywhere outside the prostate.
Also, my research had told me that a bone scan was recommended
for
patients with cancer of my grade. The
nurse’s response was that that they never do PSMA-PET scans and
insurance would
never cover it. I guess they assume they
don’t need the PET scan if they’re cutting out the prostate, but this
was another
disappointment.
After a couple hours of these preliminary
meetings, the
surgeon arrived with a couple assistants.
He spent, perhaps, 90 seconds in the office with me. There would be no chance for me to ask all
those questions I had prepared and certainly no discussion of anything
but
surgery. He did assure me that he would
be able to take good care of me and added that the urinary frequency
due to my
enlarged prostate would no longer be a problem—since I wouldn’t have a
prostate
any more. In retrospect, I probably shouldn’t have expected any
more
time with the doctor as I understand he is busy performing
hundreds—maybe even
thousands—of prostatectomies a year.
After the doctor was finished with me, I was
ushered to
another room to meet with a woman whose title escapes me but who I
would
describe as the “closer.” Her job was to
give me the medical orders for things like a chest x-ray and 3D MRI
that I
would need to get before the surgery.
She also provided a checklist of other clearances I would need
from my
cardiologist (which I had actually gotten a couple days before) and my
primary care
physician.
Her job was also to get me to sign all the authorizations for the surgery so it could be scheduled, even though I had told the nurse that brought me there that I was still undecided about what I would do. When I told “the closer” I was undecided and wanted to look at other options, she did not seem happy. I believe she warned that not signing now could delay my surgery date. At this point, I honestly felt like I was being sold a timeshare rather considering a medical procedure.

So I walked out of the building with a list of
things to get
done and a brochure about the Da Vinci machine that would be used in
the
surgery. Thinking about the appointment
on the drive home and thereafter, I felt a bit lost.
I really hadn’t gotten any new information.
I did have the genetic test scheduled and
they gave me a location where I could get the 3D MRI, so those were
good things,
but I really didn’t get any of my questions answered.
Nothing about the situation felt right but I
had no idea where to look for other options.
Who could I find to answer that list of questions I still had? How could I find a radiation oncologist that
I could trust to give me good information about that option?
On my drive back on Route 528, I had the idea of
calling my
brother, John, who was down from Rhode Island and staying in Cape
Canaveral for
a couple months. I felt like talking
about my day with someone who had been through prostate cancer before. When he said he and his wife, Carol, and
their son, Andy, were just hanging out on the beach, I drove over. It felt good to vent a little bit about my
somewhat disappointing appointment.
Verbalizing my concerns helped me focus on starting to come up
with a
plan to address my concerns.
Despite my indecision about my treatment, I still
started
working on completing the items on the checklist I had been given. I figured I’d need to get an MRI no matter
what I decided. Also, I had already had
a cardiologist appointment a couple days before meeting the surgery
team and my
cardiologist had signed off on my going off blood thinners prior to
surgery, so
that was done.
After the AdventHealth appointment, I went to Neuro Skeletal Imaging in person with my orders to schedule an MRI and chest X-ray. This facility had been recommended by AdventHealth since they had a 3D MRI imaging machine. It was called a 3-Tesla machine or something like that and I remembered hoping it had nothing to do with Elon Musk. I wasn’t sure if this machine would do a multiparametric MRI (mpMRI) as I had read about and the staff at Advent didn’t seem to know what I was talking about. I assumed it would be fine as it would be a 3D scan and the name sounded cool enough.
A day or two after the appointment, I answered a
call at
home that showed it was from AdventHealth, thinking it was a follow-up. I guess it was, in a manner of speaking. The gentleman on the line had a heavy
island-sounding accent and proceeded to tell me what a great surgeon I
had and
how lucky I was to get him. I replied
that yes, I knew he was world-renowned and I knew people that had used
him. He essentially kept repeating how
great the surgeon was and I kept agreeing, wondering where this
conversation
was going. This, again, felt like a
sales job rather than a discussion about a medical procedure. Eventually he asked if I was a “man of
faith.” When I replied that I was not
the conversation soon ended. I kept
thinking how strange that call was.
I had noticed that the screen savers on all the computers at
AdventHealth all displayed biblical verses, which I thought a little strange. I didn’t remember seeing anything like that
at any other health care facility I had been to. I only realized after the fact that the
hospital was actually founded by Seventh-Day Adventists (hence the name, as light
dawns on Marble-head me) and was, in effect, a Christian ministry. I guess that’s not unusual as many hospitals
seem to have religious roots. With
regard to health care, I wouldn’t think that was good, bad or indifferent, but
I thought it was interesting and likely explained the phone call and reaction
of the caller.
Another couple days later I received an email from
the
surgical coordinator. The email was also
strange in that, amongst the reminders about the checklist of actions I
had to
complete, smiley-face emojis were sprinkled.
It might be a sign that I’ve gotten old and cranky that smiley
face
emojis in a message about prostate surgery somehow annoyed me.
I replied politely that I had scheduled things
like the MRI
and x-ray but that I was still undecided as to my final course of
action. She replied, amidst more
smiley-faces, that I
should let her know once I had decided.
Apparently, she didn’t really want to know if I had decided
against the
surgery because, when I told her that a month and a half later, she did
not
reply.
A couple months later I got a rather mean-spirited
letter
from Advent Health, chastising me for not completing my pre-surgery
tasks,
stating they tried to reach me many times (they hadn’t) and telling me
I would
now have to start the whole process all over again.
I was puzzled—and a little pissed off—but it
kind of reaffirmed my feelings about that whole situation.
At some point shortly after the AdventHealth
appointment, I
had sort of a mini-revelation. What if,
instead of going for the most convenient or cheapest method of treating
my
cancer, I looked for the BEST place to get it treated.
Even if it meant traveling out of town or
choosing a treatment method that most would not choose.
What if I didn’t worry about cost and did
what my gut told me was the best choice for me?
At that point, I started looking at the most
well-known
cancer treatment centers, like Moffit in Tampa, but then had the better
idea of
specifically looking for the best prostate cancer treatment centers in
the
country. I eventually came up with about 5 that were on most lists:
Orlando
AdventHealth (where I had already been), Johns Hopkins in Mayland
(where
prostate cancer pioneer Dr. Walsh had practiced), Sloan Kettering in
New York,
Dana-Farber in Boston and, I believe, Mayo Clinic in Jacksonville,
Florida. I looked at all their websites
and tried to
determine which had all the latest technology I had read about.
As I did this research, I started thinking about
my 35 years
living in Florida and came to the realization that anyone I had hired
to do
anything in Florida—from landscaping, to irrigation repair, to fence
installation—was incompetent. Okay,
that’s probably an exaggeration, but it is, at least partially, why
I’ve tried
to do so much of this type of stuff myself—despite the fact that I am
NOT
“handy” and mostly quite incompetent myself. Still,
my thinking went, if I can’t trust
anyone in Florida to weed whack my yard can I find a Florida man (or
woman) I
trust to cure my cancer? If they were
the best at what they did, wouldn’t they be working in New York or
Boston or L.A.
or somewhere like that??
My thought process
led me to Dana Farber Cancer Institute in Boston. I
was very familiar with Dana Farber because,
unfortunately, I have had many relatives and friends who have had
cancer. Those who were treated at
Dana Farber had
only positive things to say about it.
Further, when my good friend Mike was at Dana Farber with
terminal brain
cancer, I spent a day with him and his wife and got to see first hand
what
excellent care he was receiving. They
didn’t even get upset when he kept hitting the nurse call button,
thinking it
was the button that would rewind a TV program on his DVR.
Several who ultimately lost their battles with cancer named Dana Farber as the charity to which memorial donations should be directed. Because of those donations, I had read a lot about Dana Farber in the newsletters they had sent over the years. More importantly, they had the latest prostate cancer technology I was looking for. Also, with Dana Farber being located in my home state, I might even be able to connect with friends and relatives still in the area if I decided to get treated there.

So I decided to try calling Dana Farber. Honestly, I figured they would not take me as
a patient, since my cancer was unremarkable.
I assumed it would be a difficult facility to get into, given
its
world-class status. I also thought my
insurance
would be unlikely to work out of state, making it cost-prohibitive. Still, I called to see what they would say.
I was amazed how efficient the phone call was. After initial collection of my information, I
was transferred to an insurance specialist who looked up my insurance
and
quickly determined that Dana Farber was in my plan.
I then spoke to a scheduler to whom I
explained I would be coming from Florida so it would be great if my
consultations could be set up within a day or two.
Later that day, they called back and had set
up three appointments with a urological oncologist, a surgeon and a
radiation
oncologist, all on the same day and just a little over a month away.
I couldn't believe how quickly this had all
transpired. With a single phone call, and
within a single
day, I had a set of appointments at a top-notch cancer facility. Better still, my insurance would cover those
appointments. So I was really doing
this. I was flying up to meet with
doctors at Dana Farber to try to figure out what to do.
Now, I could have a discussion with doctors
who could give me a complete picture of my treatment options.
I still had over a month to think about all this and get ready for the appointments. I decided to continue completing some of the actions required for the surgery, in case I went that route. Also, I was anxious to finally get some scans done on my cancer and figured they would be useful no matter what course I pursued. Plus, I had already scheduled my MRI and chest X-ray.
I also talked to my brother John and, even though he and
Carol would be getting back from Florida just a few days before I arrived, he
said I could stay with them and my nephews at their house in Rhode Island when I
came up for my appointments. With that
part figured out, I booked my flights and rental car. I believe John offered to drive me up to
Boston, but I didn’t want inconvenience him any further. Because I was taking this unusual step of travelling over
1000 miles to talk to some doctors when, one would think, there must be fine
ones in Florida, this felt like something I should do myself.
Shortly after making all the appointments, my godmother, Barbara, passed away in Massachusetts. As I was never going to miss her funeral, that meant rescheduling my MRI. Luckily, they were able to give me an appointment just a week later. As it turned out, this trip would be the first of many that I would take to New England in 2024. (I’ve written about the funeral trip here).
While waiting at Logan airport for my flight back from the
funeral, I decided I needed to do more preparation before my appointments at
Dana Farber the following month. I found
another current book on Amazon, “Prostate Cancer 20/20” by Andrew Siegel, and started
reading it immediately. A lot of the
information just reaffirmed what I had already read, although there were some
new points. I was excited to see a
chapter entitled: “Should I Have Surgery or Radiation?” Unsurprisingly, the chapter does not
explicitly answer the question but gives a lot of detail about the pros and
cons of each. So I had more information
but was still undecided about what would be best for me. I looked forward to the Dana Farber
appointments to help me make that decision.
A week after getting back from the funeral, I had
my
appointment for the MRI and chest X-ray at Neuro Skeletal Imaging (or
just NSI
as they apparently prefer to be called, likely due to some corporate
rebranding
that says every company needs to go by an acronym rather than words). The scans went fine and, if I remember
correctly, as I had requested, they even played some songs by “The
Offspring”
in my headphones during the MRI.
I had requested a CD with the images so I could
take it to Dana
Farber (or wherever I wound up being treated).
I repeated the request again after my last scan and was told to
wait in
an interior waiting room. I was
apparently forgotten about as I was waiting for maybe 20 minutes or so. When someone saw me, they asked what I was
doing there. Apparently, almost everyone
had gone to lunch. When I said I was
waiting for my CD, they quickly produced it and I was on my way. Weeks later I would find the CD only
contained the chest X-ray and not the MRI.
Maybe they would have burned the MRI to CD after lunch.

When I originally scheduled my Dana Farber visits,
all three
of my appointments were supposed to be the same day, in the same
location. However, a few weeks before my
trip, they
called to say my appointment with radiation oncologist Dr. Kim needed
to be
changed. Now, I would be seeing another
radiation oncologist, Dr. Sayan, but it would be on Wednesday at the
Yawkey
Center in Brookline. I was annoyed, as
this meant having to drive into Boston twice, with the second trip
deeper into
greater Boston and in morning traffic to boot.
Also, I’d have to change my travel arrangements, but there was
really
nothing I could do and I was still looking forward to talking to Dana
Farber
doctors. As it turned out, the change of
doctors might have played a crucial role in my ultimate decision.
I started flying Southwest airlines years ago,
largely
because of their nonstop flights to secondary airports like Manchester,
NH, and
Providence, RI—my destination on this trip.
Another reason I’ve liked Southwest is because they always let
you
cancel or change flights without penalty (now, it seems they all might
do
that). So, I was able to easily change
my return flight with no cancellation fee, although the later flight
did cost
about 50 bucks more. It was easy enough
to add a day to the car rental. And, as
it turned out, I could get another day of luxury accommodations at my
brother’s
house at no additional charge.

A couple weeks after the trip changes, the day to
leave
arrived. For some reason, this particular
trip wound up being dotted with minor technical issues.
The first occurred when I was going through
security screening in Orlando. My
printed boarding pass would not scan—maybe my printer had been low on
ink.
I’m sure I got a lot of eye rolls from young folks
looking
at the old guy with a paper boarding pass.
For a second, I worried I’d have to go back and print out a new
boarding
pass at a kiosk, then get back in line.
There was a long line, so maybe I’d miss my flight, not get
another one
and miss all the appointments. Luckily,
I had the Southwest app on my phone and was able to step out of line,
fumble
through it while holding my bags, bring up my boarding pass and get
through
security. Crisis averted.

I had brought the CD which, allegedly, contained
my MRI
images and the chest X-ray that the surgeon had asked for.
However, when I actually looked at the CD after
I got to Rhode Island, I realized the label only said “chest x-ray” on
it. After borrowing a USB CD drive from my
nephew,
I was able to determine that, indeed, the imaging facility had left the
MRI off
the CD. Had I bothered to look at the CD
at any point between the day I received it and when I left on the trip,
it
likely would have been very easy to get a new, correct CD.
Now, I was over 1000 miles away and realizing
I would have no images to provide to Dana Farber before my appointments. There’s probably a lesson in there about why
I should double check stuff and not assume other people did things
correctly.
It was Sunday when I realized the problem, so I sent an email to NSI, the imaging facility, and also left them a voice mail. To their credit, NSI overnighted a corrected CD to my brother’s home and I was able to deliver it to Dana Farber before my Wednesday appointment. Ultimately, Dana Farber did their own imaging, so I’m not sure if they actually needed my CD, but at least I did get it to them.
I flew into Providence the Sunday afternoon before
my Monday
appointments. I didn’t have to be there
until the afternoon but I wanted to account for potential traffic and
my
possibly getting lost. I certainly
didn’t want to risk being late after travelling all this way. John drove me to the north side of Providence
to pick up my rental car around 10am (more about the car later).
My first two Dana Farber appointments were at the
Lifetime
Center in Chestnut Hill, where Boston College is located.
My knowledge of the west side of greater
Boston was not great, but I had been to Chestnut Hill for a Boston
College
football game with my brother John in 2008, shortly after our mother
died. His son Daniel, my nephew, was going
to school
there at the time. I remember taking the
MBTA subway in and walking to the stadium on that wet fall day. BC beat Rhode Island pretty easily.

My return trip to Chestnut Hill, 15 years after
the BC game,
was a surprisingly easy drive. After
picking up my rental car in North Providence, I got right on I-95 and
got to my
exit in less than an hour. That was even
after stopping at the first rest area to figure out how to work the
radio and attempt
to control the heater.
The facility was just a few miles off the
interstate. Too close, as it turned out,
as it came up on
me before I was looking for it and I blew right past it.
Further, the place was on Route 9, a divided
highway with no U-turns. I had to circle
back around on side streets to finally get to the facility. Turns out, leaving early for my 12:15pm
check-in time was a good idea. I was in the free parking garage in
plenty of
time.

Upon entry, everyone was required to don a mask,
as COVID
was currently in an upswing. I checked
in, got an ID sticker and received directions to where I had to go for
my
appointments. I also stopped at the
imaging department and dropped off the semi-useless CD that I brought
from
Florida that contained only a chest X-ray and not my MRI (as mentioned
in a
prior rant). I was immediately impressed
with how efficient everything was.
My first stop was to see Dr. Serzan, a medical
oncologist. From my research, I already
knew a lot of what he was saying in his introductory comments about
prostate
cancer and treatment options. He had
reviewed my biopsy results and concurred with the finding from the
initial
reading of it, so I finally got the second opinion that all the books
recommended.

He talked about the two basic options of surgery
and
radiation. With my grade of cancer, he
recommended also getting 6 months of hormone therapy if I chose the
radiation
option. This was a little disappointing
as I had hoped the cancer was small enough to not need the hormone
treatment
and the side effects it would bring. As
I already mentioned, my father had gotten hormone treatment for his
prostate
cancer since, with his advanced age, surgery or radiation were not
advisable. I believe back then—over 20
years ago—he was given estrogen. Today,
they would use Leuprolide (aka Lupron) injections and Bicalutamide (aka
Casodex)
which, incidentally, is the drug that has been used for chemical
castration of
sex offenders. The estrogen had caused
my father to have hot flashes, but also weakened his bones which led to
a chain
reaction of other problems that I discussed earlier.
Dr. Serzan told me that I would get a Lupron shot
in the
butt (not his words) prior to radiation to stop production of
testosterone. In addition, I would be
taking the Casodex pills daily to, essentially, prevent whatever
testosterone
was left from doing anything. Together
they would starve the cancer of the testosterone that “fuels” the
prostate
cancer.
The side effects—in addition to the reason they
give it to
sex offenders—could be fatigue, weight gain, mood changes and, of
course, hot
flashes, as well as more rare, more serious stuff that most medications
warn about. Since I would be only taking
the drug for 6
months, the side effects were expected to dissipate over time. Dr. Serzan would be monitoring my bloodwork
and general health during hormone treatment, if I went that route.
I still had that big document with all my notes
and
questions—in fact, it was likely bigger and had more questions than
before. Unlike my Orlando appointment,
Dr. Serzan was perfectly willing to stay as long as needed to answer
all my
questions. I think I might have been in
his office for an hour.
My next appointment, later that afternoon, was with Dr.
Wollin, a surgeon. I was already leaning
towards radiation, assuming the radiation experts told me it was feasible, but
I wanted to get as much information about all options before finalizing any
decisions.

Interestingly, Dr. Wollin said he was flattered
that I was
talking to him, since he had seen that I had met with, perhaps, the
most
world-renowned prostate surgeon in Orlando.
As with Dr. Serzan, his introductory statements about prostate
cancer
were mainly things I already knew from my research.
In response to my question about potential
side effects of surgery, he indicated that different surgeons had their
own
particular techniques, each of which might work better to prevent one
side
effect or another. This was new
information for me as I kind of assumed all surgeons did pretty much
the same
thing. Maybe if I had watched those
cringe-worthy prostate surgery videos I might have known better.
We also discussed logistics, such how long I would
need to
stay in Boston should I chose to have surgery at Dana Farber. As had been the case with Dr. Serzan, I
probably spent close to an hour with Dr. Wollin. He
answered all my questions and was willing
to spend as much time with me as I needed—unlike the world-class
surgeon in
Orlando.
After my appointments, I had planned to accompany my brother, John, to one of his presentations to promote his hiking book, Walking Rhode Island, that evening. This one would be for the Cumberland Land Trust in Cumberland, Rhode Island. Between the length of the appointments and the traffic coming out of Boston, it looked like might not make it back to Rhode Island in time to join him. I called John from traffic and gave him my Kia nav system-provided ETA and he said he would wait for me. So I made it back to his house in time to grab a snack (I hadn’t eaten since breakfast) and jump in his car to get on the road again. In addition to supporting his presentation, I was wanting to discuss what I had learned from the day’s appointments.
John’s presentation went off well, as usual, and
was
well-attended. I helped with setup and
book sales, which were quite brisk. A
big surprise was that my cousin Kim and her husband, Kevin, had driven
down
from Massachusetts for the event. It had
been I-don’t-know-how-long since I had seen them and it was great to
talk to
them. Many years ago, Kevin had gotten
radiation treatment for testicular cancer and, since I said I was
considering
that route for my prostate cancer, he offered to share his experiences
with
me. I took him up on that offer and we
had a long, very helpful phone chat a few weeks later.
 |
 |
My brother John's book, "Walking Rhode Island"
|
I accompanied John to a book
presentation in Cumberland, Rhode Island
|
After John’s presentation, we were able to find an
open
restaurant and I finally got to eat.
This being New England, I asked if they could put the Bruins
game on one
of the TVs. I was disappointed that they
were losing by 3 goals, but happy to talk through the day’s events with
John. As always, he was supportive of my
approach
of getting information before deciding what to do.
Because of the movement of one of my appointments
from
Monday to Wednesday, Tuesday was a “day off” for me.
I took advantage of the day by going on a
somewhat chilly morning hike with John and some of his friends to the
Barn
Island Wildlife Management Area on the Connecticut coastline. It was a really interesting 4-plus mile hike
through a
marsh and wooded areas, winding up along the coast.
You can read John’s article on the hike here.
 |
 |
 |
Overview of Barn Island Wildlife Management Area
|
John taking notes along trail through marsh at Barn Island
|
View of ocean across the marsh at Barn Island |
 |
 |
Babbling brook in the woods at
Barn Island
|
View of
marshes at Barn Island
|
 |
 |
View across Little Narragansett
Bay at Barn Island Wildlife Management Area
|
Swans in the ocean at Barn Island
|
 |
 |
Me looking out over Little
Narragansett Bay at Barn Island
|
On the way home we saw this house
that looked like a castle
|
The hike was a nice start to a day which turned
frustrating
as I dealt with the third technical issue I ran into on this trip. This one involved my rental car.
To save some money, I had booked the
“Manager’s Special” at a Hertz location in North Providence. Renting a car at the airport which would have
cost over twice as much.
I figured they’d give me the cheapest, crappiest, smallest
car they had, which would be fine with me—even if it was a Yugo or a Chevette
or something. I was surprised—and a
little excited-when I arrived at the rental place to find I was actually
getting an EV, a Kia EV6. The rental
folks assured me that there were lots of places where I could get it
charged. I would need to get it charged
because it was unlikely to make it to Boston and back twice on a single charge. Plus, they would charge me $35 if I returned the
car not fully charged.

Once I figured out how to operate the car, it was actually
pretty fun to drive. I did have to stop
at the first rest area I saw to figure out how to turn the radio on and to try
to control the heat. I never actually
got the heater under control as, despite setting it to what should have been a
comfortable temperature, it was either blasting scalding hot air or leaving the
car freezing cold (this was March, so still technically winter).
The real problem came the day after my first appointments when
I tried to get it charged. At first, it looked like it would be easy as
Google showed me several charging stations that should work right in Cranston
where my brother lived. However, when I
talked to my nephew Andy, who actually has worked in the EV industry, I found
things would not be that simple.
As it turns out, the charging stations available locally
were of low kilowattage, meaning it would take at least overnight to fully
charge the car. There would be no way to
fully charge it before I would need to leave for Boston in the morning. I had thought that the worst case would be
that I would run a long extension cord from my brother’s garage or house and
get some juice into the car that way.
But that would have taken even longer and would only work if you
had a special adapter, which I, of course, did not have.
Conceding that I was going to have to pay the $35
not-fully-charged
fee no matter what, my brother, my nephew Andy and I set out to a local
charging station to at least get the car enough charge for me to return
to Boston and get back. My next surprise
was that you couldn’t just insert your credit card and start charging your
car. In fact, I thought it might just
work by plugging it in since this particular charging station was affiliated
with a local utility which advertised that the first 2 hours were free.
I couldn’t have been wronger about any of that. The only way to work the pumps was through an
app created by the company that owned the station, Chargepoint. So, while parked at the pump with my rental
EV, I downloaded the app on my clunky old phone, set up my account and entered
my credit card info. Now, I thought, I
could charge the vehicle.
I was mistaken yet again.
Shortly after all that effort I found that I needed to
enable Near Field Communications (NFC) on my phone. NFC is used to facilitate tap-to-pay
technology on a smart phone. That would
be great, except that my phone was 7 years old and did not have NFC. So Chargepoint let me download and install an
app that could never in a trillion years work on my phone. Andy was helpful, but I think he was probably
really amused or really disgusted by his uncle’s apparent technical
incompetence.
I had heard about Chargepoint from watching CNBC, the “stock
market channel.” I knew their stock had quadrupled
amid EV hysteria after the company became public but had since lost over 90% of
its value and was approaching penny stock territory. Having now had this first-hand experience
with the company, I realized why they are on the verge of bankruptcy and why
they probably deserve go out of business.
Their software might have been developed by grade school dropouts who
don’t have any idea about a basic programming concept that you should check
whether the program could even work on the device on which it is being
installed. They could have had my money (and
I wouldn’t be writing this rant) if their charging stations just took credit
cards, but they designed a system that made it absolutely impossible for me—and
likely many other potential customers—to use their product.
 |
 |
In order to attempt to charge my rental EV, I had to deal with Chargepoint, the company that runs the local charging stations
|
Chargepoint stock has plummeted and, from my experience, I can see why
|
But I digress.
I felt I had been defeated by “technology,” so we headed
back to my brother’s house. Andy said he
had found a faster charger at a Walmart about a half hour away. It would cost about $50. Instead of pursuing that idea, I called the
rental car place to ask if they could charge my car just a bit if I brought it to
them. They said they could not do
that. As calmly as I could, I explained
that I simply had no way to charge this car, which meant I couldn’t get to
Boston for my doctor’s appointment. I
asked if I could bring it in and swap it for a good old-fashioned gas-powered
car. I said I’d pay whatever fee and
price difference they saw fit to charge me.
They put me on hold, then came back and told me that, if I brought the
car back by 5pm (it was about 4), they’d swap it out with no additional
charges.
So I battled the traffic, got across town and brought the
car back. Waiting for me was an internal
combustion engine, several-years-old Toyota Corola that they had not had a
chance to clean yet. It was a beautiful
sight. While there, the manager showed me
how they charged their EVs. They had one
plugged into the wall with an extension cord and that special adapter. He said it took them 2 days to get the car
recharged. He also said the “Manager’s
Special” was almost always an EV. I’m
guessing that offering to rent EVs for really low prices—and not telling the
customer they’re getting an EV—is the only way they can ever actually rent one.
After I was able to swap to a car with an internal
combustion engine, the day improved. We
all had a nice dinner at Avvio Ristorante, one of Cranston’s best restaurants. A friend of Andy’s had said they had the best
scallops in town and they were probably right.
So ends my quite long digression from my initial appointments at Dana Farber.
 |
 |
My Wednesday appointment was at 10am, so I left Rhode Island
around 7, again fearing traffic, getting lost, etc. This time I would have to go pretty deep into
Boston. I also had to make a stop back at
the Lifetime Center, where I had been Monday, to drop off the CD that had been
overnighted to me by the imaging people in Florida. This CD actually included the MRI as it was
supposed to.
The drive up I-95 to Route 9 (again) was pretty smooth, but getting
to the actual facility was more difficult.
First, the left turn I had to take was onto Brookline Ave, a busy street
that leads to Kenmore Square and basically goes right by Fenway Park. I didn’t realize the left turn lane was
backed up a long way and found myself in the wrong lane, well past where I
should have gotten in line. Amazingly,
someone let me cut in line in front of them¸ saving me from attempting an ugly
U-turn or otherwise figuring out how to get where I needed to go. Maybe this was a sign omens were turning good:
yesterday I was able to resolve my rental car issue and today a reputedly
ruthless Boston driver took pity on a confused person with out-of-state plates.

The next obstacle was the semi-gridlocked traffic right in
front of the Yawkey Center. I eventually
worked my way into the garage and to the parking valet still with time to
spare. One of the few negative
experiences at Dana Farber was with the valet parking cashier on my way out. They were quite rude and unaccommodating of
people like me who had no idea where they were going (or what they were
doing). I self-parked the next time I drove
to this facility.
I mentioned the radiation oncologist I was originally supposed to see Dr. Kim but I wound up seeing Dr. Sayan. Dr. Kim probably would have been great also, but I took an immediate liking to Dr. Sayan. In my career I worked as a software engineer on large teams and even interviewed potential employees. I think I developed a sense for those who truly liked their work as compared to those there just there to get a paycheck. Dr. Sayan was extremely knowledgeable, as one would expect, but I could tell he also really enjoyed his work and was dedicated to it. I was quickly getting a good feeling about the route I hoped to take.

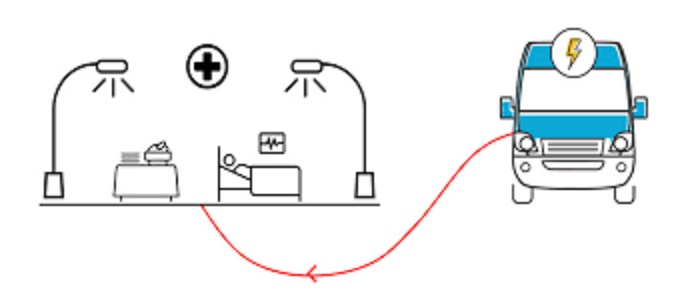
He explained that, if I chose to be treated with External
Beam Radiation Therapy (EBRT or, as I generally refer to it, “radiation”), it
would take about 5 and a half weeks.
This was a bit disappointing, as I had read of other radiation methods
that could complete treatment in much shorter timeframes. Still, this was better than the 9 weeks of radiation endured
years ago by the two people I knew who had been through it: my brother and a
former co-worker. Dr. Sayan explained
the other methods that I asked about were too new or risky for him to
employ. He also mentioned each treatment
would take only a few minutes.
Dr. Sayan also mentioned all the potential short and long
term side effects of radiation that were becoming familiar to me: things like fatigue,
urinary frequency, weak stream, having to poop more (not his words), and
impacted sexual function.
He also affirmed that radiation had been found to be just as
effective as surgery as a cure for prostate cancer. More important to my situation, Dr. Sayan
said my particular cancer could be cured with radiation. This was one of the key questions I wanted
answered.
As we talked about radiation treatment, it was becoming
clear to me that Dana Farber/Mass General had all the latest technology that I
had read about. They would use
image-guided radiation, meaning, essentially, a picture would be taken before
every treatment to ensure the radiation would be directed to the correct
location. This handles situations where
the prostate might have moved between imaging and treatment. To facilitate the imaging, tiny gold markers,
or fiducials, would be placed in the prostate prior to treatment. That made me think that anyone can get
gold-plated teeth but a gold-plated prostate sounded really bad-ass.
 |
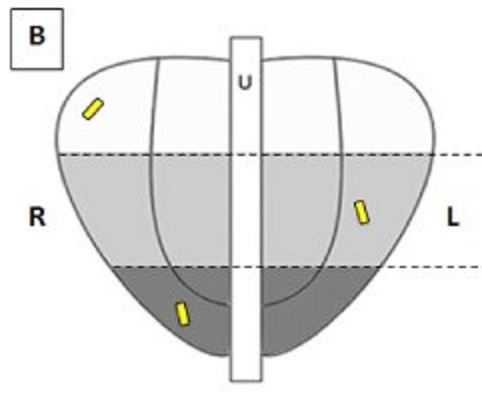 |
Dana Farber also had the latest imaging technology,
including a special 3D machine that would “map” the prostate prior to
radiation. Apparently, these images
would be more detailed than the ones I had gotten in Florida. Dr. Sayan indicated this mapping would be
done about 2 weeks prior to starting radiation, meaning the images would capture
any recent changes that might have taken place in my prostate. The gold fiducial markers would be inserted
around the same time. He explained he
needed those two weeks to design a radiation plan tailored for me. That sounded impressive: my own personal
radiation plan.
Earlier I mentioned I had read about the importance of a
PSMA-PET scan, which uses a newly developed machine to find prostate cancer
anywhere in the body. The great thing
about this type of scan is that it detects whether the cancer has spread
outside the prostate. If it has,
treatment would be more difficult with more limited options and less hope for
successful cure. Having this information
up front, rather than being surprised later, seemed pretty critical to me. I wondered if such a scan, if it had existed
back then, might have benefitted someone like my brother Walt who had a
prostatectomy but still had to undergo radiation 5 years later when the cancer
showed up again.
Prior to invention of the PSMA-PET scan, a bone scan was
typically done. The problem with that is
that it doesn’t do a good job distinguishing between prostate cancer and
arthritis. When I talked to a former
co-worker who had undergone radiation treatment for prostate cancer years ago,
he mentioned that he’d gotten a scare after his bone scan “lit up” in several
areas. The initial worry was that the
cancer had spread all over but, in fact, the scan was just showing
arthritis.
I told Dr. Sayan that, when I had asked about a PSMA-PET
scan at the Orlando facility that I visited, a nurse responded that they almost
never did them and insurance would never approve one. He responded by assuring me that he could get
the scan approved. It probably helps
that, unlike other treatment facilities, Mass General actually has all this
equipment in-house and doesn’t need to send patients to an outside location.
The machines actually used to deliver the radiation would also be state-of-the-art, allowing much better targeting of the cancer without unnecessarily radiating other areas. For further protection, they would use SpaceOAR, a substance that is injected to buffer the rectum from radiation. The SpaceOAR dissipates over time after it has done its job. This was another protective measure I had hoped would be used if I chose to receive radiation treatment.
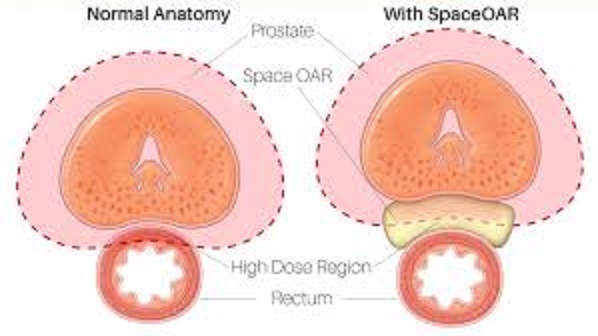
In sum, everything I had read about, from the imaging to the radiation and protection from damage, could and would be used by Dana Farber to treat my cancer.
Dr. Sayan and I also talked at length about the 6-month hormone
treatment that he recommended for a Grade 3 prostate cancer like mine. I had already read about the side effects and
discussed them with Dr. Serzan, as well.
Dr. Sayan said that, if I wanted and was found to be eligible, I could
enter a clinical trial that was testing a different type of hormone treatment
drug. This other drug is typically given
to patients in more dire situations where the cancer can only be slowed and not
cured. However, it does not generally
produce the side effects that standard hormone treatment does. The trial is trying to determine whether this
other drug could be effective for radiation patients also undergoing temporary hormone
therapy. I already knew that, when
signing up for a clinical trial, they essentially flip a coin to determine if
you get in the “experiment arm” or the “control arm.” In this case, it would mean getting either
the experimental drug or the “standard of care” drugs. Of course, I’ve already discussed how unlucky I’ve been at
“coin flips” when playing Texas Hold’em, so I assumed I’d get the standard
drugs with the side effects.

Spring is the worst time of year for my allergies in Florida
and, in February and March, my eyes are often runny. I mentioned earlier that, because of COVID
concerns, everyone at Dana Farber was wearing masks. Wearing a mask, with my blocked sinuses,
generally exacerbates my allergy symptoms and, during our discussion, my eyes
were watering up. Dr. Sayan thought I
was sobbing and assured me that everything would be okay. When I told him about my allergies we had a
little laugh.
As our discussion continued, Dr. Sayan seemed to get the
sense that I was strongly leaning towards radiation and we started talking
about where I could stay in Boston for a month and a half. He mentioned there was a place, Hope Lodge,
where I could potentially stay for free, if space were available. Ultimately, Pat and I decided that, rather
than the lodge, we would stay in a hotel, but Dr. Sayan’s telling me about the
lodge further convinced me how much Dana Farber cares for their patients.
When I walked out of the meeting with Dr. Sayan I was pretty
much convinced that radiation treatment at Dana Farber/Mass General was the way
I wanted to go. However, there was still
a lot to think about, such as how to make sure Pat had everything she needed
while home alone. Also, how would lawn
mowing, pool maintenance and other chores get done? There would be a lot of logistics to figure
out such as where I would stay, how I would get around Boston and how and when I
would travel back to Florida during treatment.
It was pretty clear I’d need some help from friends and relatives with
things like rides to airports, putting out the trash and feeding the cats, to
name a few.
I thought about all this on the drive from Boston back to
Rhode Island. Because I had just the one
morning appointment, I had planned to meet John in downtown Providence for yet
another book presentation, this time at the Hamilton House, an adult learning
facility. After that, we could return my
rental car.
On the way back, I also had intended to return to the
Lifetime Center to retrieve the CD I had dropped off, but completely forgot
about it. It was probably just as well
that I didn’t attempt whatever U-turns would be required to get back to the
facility from the “wrong” side of the road.
Since I was increasingly sure I’d be getting treated at Dana Farber, I
figured I probably wouldn’t need the CD again. Plus, if I wound up needing it, I could likely
get yet another copy of it. Also, the
Dana Farber folks had told me the CD would be destroyed in a couple weeks if I
didn’t pick it up so I wouldn’t have to worry about a CD with my info floating
around for years. With all the doctors
and medical facilities that already had my information, this was the least of
my worries.
On my way to John’s event, Google played another trick on
me. When I was entering the downtown area
and getting close to my destination, my phone made a funny noise, after which I
eventually realized Google was routing me out of the city. When I was able to pull over and figure out
what was going on, I realized Google had changed my destination to the location
of a previous hike I’d taken with John.
After I re-input my destination and got back on track I was able to finally
get to the Hamilton House—late, as usual.
Again, John’s presentation was well-received and, afterward, I helped
with lots more book sales.
After the presentation, John followed me back to the Hertz
rental place. On the way I stopped and happily
filled the car with $11 of gas with no extension cords required. Overall, I wound up pretty happy with the
rental car place. Getting the “Manager’s
Special” EV was my mistake but they resolved the problem for me. I would actually rent a car from them again.
Before my flight back to Florida, we had a nice family
dinner at the house. I had more time to talk
to John and he was very supportive of whatever treatment option I chose, which
was looking like it would be radiation at Dana Farber.

I knew Pat would not be thrilled to have me gone for a month
and a half when I could get surgery in Orlando and be home in a day or
two. I had tried to convince her that,
if I did get treated in Boston, she could come up with me for at least part of
the time and it would be like a vacation with great restaurants, museums and
historical sites. Assuming I felt well
enough, I would have lots of free time since the treatments would only take a
few minutes each day. Further, with all
that free time, I hoped we would be able to visit with relatives and some old
friends.
After my return to Florida, I again turned to my sometimes-fickle
friend, Mr. Google, this time to locate a French restaurant. I found one, a rebranded higher-end place aptly
titled “Le French.” I figured a nice
dinner of Pat’s favorite cuisine might be the appropriate place to discuss my
treatment decision. Over dinner we
talked over the whole thing, from the reasons I wanted to do this at Dana
Farber to potential logistics of my being away for 6 weeks. In the end, Pat probably still would rather I
was treated locally, but she respected my decision and would make the best of
it. And we wound up finding a new
favorite restaurant that we have visited many times since then.

| Home |
Previous |
Next |